In emergency settings, recognizing critical signs and symptoms quickly and confidently allows you to take swift action to save lives and preserve the quality of life for those under your care. Becks Triad is one such set of symptoms. It can help diagnose life-threatening conditions like cardiac tamponade. In this guide, I explore this triad, what to do when you see it, and how to avoid its limitations leading to an improper diagnosis.
What is Becks Triad?
Becks Triad is a set of three clinical signs that indicate your patient may have a serious heart condition called a “cardiac tamponade.” If your patient has this, then fluid is building up (effusion) around the heart, pressuring it and preventing proper pumping. Knowing how to spot possible cardiac tamponade is crucial because it can signal that your patient has a life-threatening condition that requires immediate action.
Cardiac Tamponade vs. Pericardial Effusion
These two terms may be used interchangeably in this guide but have slightly different meanings. Pericardial effusion is the accumulation of fluid in the pericardial sacs. Cardiac tamponade refers to the cardiac compression that results from it. (USCF.edu)
What Are the Three Beck’s Triad Symptoms?
- Hypotension: When excess fluid compresses your patient’s heart, it can’t pump blood effectively, leading to a drop in blood pressure.
- Jugular Venous Distension (JVD): This tells you that the blood isn’t returning to the heart as it should. Fluid buildup prevents normal blood flow as well.
- Muffled Heart Sounds: The fluid around the heart muffles the sound of heartbeats. It’s like trying to hear a drum that’s being played underwater—everything sounds quieter and more distant.
These are often accompanied by patient-reported chest pain and shortness of breath, the most common other symptoms.
Do You Know What to Do in This Scenario?
Imagine you’re a paramedic arriving on the scene of a serious car accident. The patient is complaining of chest pain, and you can see that they can’t catch their breath.
As you assess them, you notice they have very low blood pressure. Upon inspecting their jugular veins in the front of the neck, you notice bulging. You then listen to their heart and heart with a stethoscope. You don’t hear the usual clear rhythm of a heartbeat, regular or otherwise. It sounds like you’re hearing the beat through an insulated wall.
You recognize this from your training. That means your patient may have cardiac tamponade. Someone must act fast to alleviate the pressure on the heart. What do you do next?
When you get an ACLS certification, it equips you with the knowledge and skills to effectively manage cases involving Beck’s Triad and many other emergencies. You can become confident that you’re prepared to provide the best possible care in any emergency and work with a team of rescuers to save a life.
Who is Claude S. Beck?
Beck’s Triad is named after Claude Beck, MD, a cardiologist who lived and worked in the mid-20th century (1894–1971). He was a pioneering cardiac surgeon who helped the field become what it is today. He introduced novel procedures such as Beck I and Beck II to improve blood flow in his patients. He trained and inspired many with what he had learned during his practice. His work became the foundation of modern cardiovascular surgical procedures and resuscitation methods.
Fun Fact: He performed the first-ever heart defibrillation.
Most relevant to the discussion today, he identified and described the signs of cardiac tamponade, which would later be known as Beck’s Triad.
What Causes Beck’s Triad?
The primary cause is cardiac tamponade from an accumulation of fluid in the pericardium (pericardial effusion). This fluid-filled sac typically protects the heart. But in this case, something is causing too much fluid in the sac. Like an overzealous security guard, it’s causing more harm than good.
What Causes this Fluid Build-Up?
- Trauma: Blunt or penetrating injuries to the chest can cause bleeding into the pericardial sac, leading to cardiac tamponade. Your patient who was just involved in a car accident may have suffered this kind of trauma. Falls and violent injuries could also cause it.
- Pericarditis: This inflammation of the pericardium is often due to infection or autoimmune diseases. As your patient’s immune system attempts to fight off the invaders—real or perceived, the pericardium accumulates fluid, causing the compression.
- Myocardial Rupture: This is a rare but severe condition where your patient’s heart muscle tears, usually after a heart attack or significant blunt trauma, allowing blood to leak into the pericardium and resulting in tamponade.
Risk Factors and Prevention of Becks Triad
Risk factors align with the causes of fluid build-up around the heart. Understanding each factor can help you put the pieces together faster. Some questions to ask as you assess the patient include:
- Has your patient recently experienced blunt or penetrating trauma to the chest?
- Do they have any known medical conditions like autoimmune disorders, pericarditis, recent heart surgery, or myocardial infarction (heart attack)?
- Have they undergone invasive procedures like a heart cath?
You should also ask if they’re showing signs of dehydration. You’ll find out why a little later.
What is Beck’s Triad Prevention?
If you are advising patients on how to prevent cardiac tamponade, consider steps that can reduce the risk of developing this condition, such as:
- Attending regular check-ups after surgery or a cardiac event
- Speaking with a doctor if they have a history of cardiac or autoimmune disorders that could lead to cardiac tamponade
- Protecting the chest from trauma in sports, recreation, home improvement projects, and work-related activities
- Getting prompt medical attention after chest trauma or a cardiac event
In Save a Life’s ACLS training course, you learn how to identify early risk factors. This training equips you with the knowledge to recognize early warning signs of this and other life-threatening conditions. This allows you to take proactive steps to prevent events, educate patients, and efficiently manage these conditions.
You can download a helpful free app called Medicode to keep your medical algorithms handy in your pocket.
Why Is Beck’s Triad Important in Nursing?
So, you’re a tech-enthusiastic, patient-centered nurse. Why is understanding Beck’s Triad critical to your practice? It allows you to identify a potentially deadly condition in your patients so that you can work with your medical team to take appropriate actions.
Early recognition is key. And often, you’re the one who spends the most time with the patient. You’re more likely to notice something wrong when checking in on your patients.
When you take an ACLS course free online, you learn how to perform a comprehensive assessment using the monitoring tools and visual assessment skills available to a nurse in a clinical setting. You learn how to make quick and confident decisions about patients in your care and how to coordinate life-saving care with your medical team.
How to Assess Becks Triad in EMS
As a paramedic in a high-stress environment, your ability to quickly assess patients based on sets of symptoms buys you vital time to get this patient the care they need.
Assessing Beck’s Syndrome in EMS in Three Steps
- Check Blood Pressure: Determine if the patient has low blood pressure (hypotension).
- Observe Neck Veins: Look for Jugular venous distention (JVD) or visible swelling of neck veins, which suggests that blood is not returning to the heart efficiently.
- Listen to the Heart: Notice if the rhythm sounds clear or muffled.
Treatment for Becks Triad in EMS
Stay Calm and Methodical: In high-stressed and often unpredictable situations, your ability to remain calm and proceed confidently dramatically changes a patient’s outcome. Follow your training and systematically rule out potential causes and complications during the assessment.
Communicate Clearly with Your Team: Be clear and concise with your EMTs and the receiving hospital. Ensure the hospital is ready to receive a cardiac tamponade patient. Make sure they are equipped to perform procedures like Pericardiocentesis (removal of fluid) or, in more severe cases, pericardiectomy (removing part of the pericardium)(NIH.gov)
Utilize ACLS Algorithms: These evidence-based decision trees will help you effectively take next steps to support your patient and manage symptoms to keep them stable.
Prioritize Transport: If you suspect that fluid is building up in the chest, stabilization followed by rapid transport to the nearest facility is crucial. The patient will need interventions and treatment you may not have in a mobile emergency care unit.
Monitor/Manage Symptoms: During transport, you’ll continue to address symptoms to keep the patient stable until they arrive at the facility.
Beck’s Cognitive Triad vs. Beck’s Triad in Cardiology
Becks Cognitive Triad is a psychology concept related to Becks Triad in name only. Dr. Aaron Beck (an American psychiatrist in the Late 20th-Early 21st Century) developed the Cognitive Triad to explain the negative thought patterns associated with depression. As a medical professional, you could undoubtedly encounter a patient experiencing these signs and may need to take appropriate actions for suicide prevention or depression treatment.
This triad of signs is:
- Negative View of Self: Your patient talks about feeling worthless, inadequate, or flawed.
- Negative View of the World: Your patient talks about the world or life as unfair, overwhelming, or filled with obstacles they can never overcome.
- Negative View of the Future: When your patient talks about the future, they use the words (or synonyms of) bleak, hopeless, or destined for failure.
These three negative views can both indicate and exacerbate depressive feelings and behaviors. If the patient dwells on thoughts like these, they may experience a downward cycle of negative thinking. This may require therapeutic intervention from mental health professionals.
Common Misconceptions About Becks Triad
I do not want to leave you with the impression that Becks Triad always indicates one condition.
In fact, according to Stanford researcher and emergency medicine physician, George, Sternback, MD, FACEP, “Subsequent studies have shown that these classic findings are observed in only a minority of patients with cardiac tamponade. However, Beck deserves credit for presenting a physiologic basis for the signs of cardiac compression.” In other words, not all patients with pericardial effusion (fluid build-up) will exhibit all three signs of Beck’s Triad. How many of these signs you see in your patient (or how subtle or severe they are) depends on the amount of fluid accumulation and its effect on heart function. (NIH.gov)
In fact, a review of two emergency department’s records found no patients with pericardial effusion had all the symptoms. And the doctors could only diagnose pericardial effusion 50% of the time based on these symptoms. This points to the need for stabilization followed by a more thorough exam before taking more invasive actions. (NIH.gov)
Subsequent research has shown that these symptoms can also appear in different conditions, such as heart failure or severe dehydration. It’s important to consider all available information before diagnosing cardiac tamponade based on these signs alone.
When you stay current on your ACLS certification while learning from anywhere on any device, you always know the most evidence-based practices for differentiating between cardiac tamponade and other conditions with similar symptoms. Continuing to advance your education with medical certifications can improve your diagnostic accuracy and enhance your proficiency with diagnostic, monitoring, and treatment technologies.
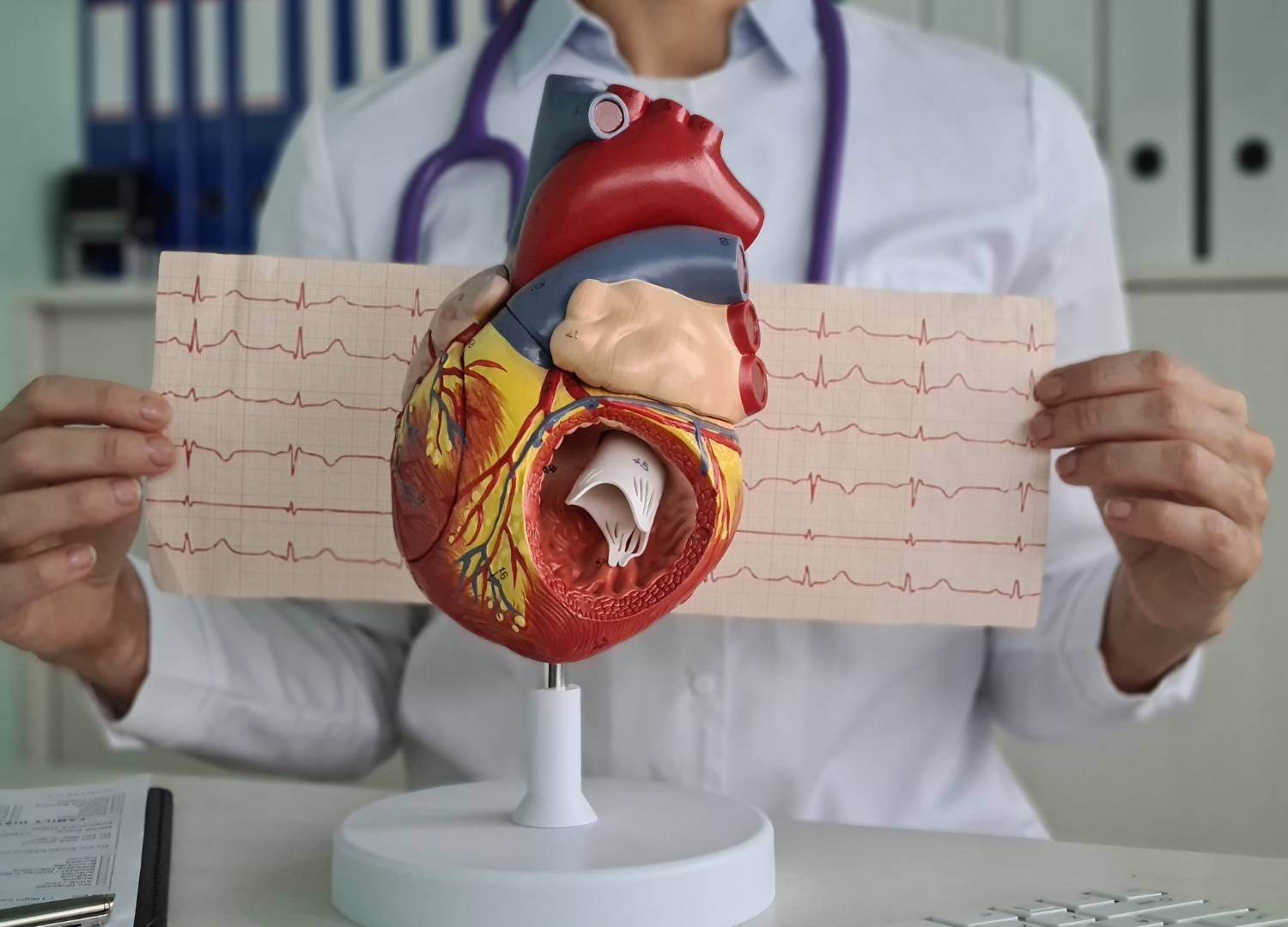
By understanding the limitations of Becks Triad, you know to use additional tests like an ECG to confirm or refute your suspicions. If an ECG shows normal heart activity, it may reduce the chances but does not rule out pericardial effusion. However, if the test reveals low voltages or electrical alternans, these may suggest there is indeed extra fluid compressing the heart. (NIH.gov)
How ACLS Certification Helps Manage Beck’s Triad
In an ACLS training course, you learn how to quickly identify and manage conditions like this within your scope of practice as a nurse, doctor, paramedic, EMT-B, physician assistant, and more. When every member of a medical team takes ACLS, they can work effectively together, applying the same evidence-based protocols quickly to save a life. Get started today!
Frequently Asked Questions About Becks Triad
Is Beck’s Triad part of pericardial effusion assessment?
Yes. Beck’s Triad is important in assessing pericardial effusion. It includes hypotension, jugular venous distension, and muffled heart sounds, which can indicate cardiac tamponade—a complication of pericardial effusion (fluid accumulation)
Is Beck’s Triad a diagnostic Feature of pericardial effusion?
Beck’s Triad alone is not sufficient to diagnose pericardial effusion. It indicates cardiac tamponade. This can result from pericardial effusion. But it’s not definitive on its own.
Is Becks Triad reliable?
It is a useful tool for starting to think in the right direction, but it will require additional testing to confirm a diagnosis. Plus, some patients may not have all three symptoms, especially if their condition is mild.







Leave a Reply