
EMERGENCY HOSPITAL CODES ARE COLOR-CODED INDICATORS used in health care facilities to alert all staff members of potential issues arising in a facility. These codes include unique prescribing criteria for how staff members should respond to a particular situation, ranging from an active shooter incident to cardiac arrest. As a result, specific statistics are unavailable for many of these hospital codes. However, some of the most notable statistics include the following:
- Active shooter incidents in hospitals have increased in frequency of one per month since 2005, reports Brown University. Across all industries, prevalence rates have risen 10 percent since 2007.
- Approximately 2,850 fires occur in health care facilities annually, asserts the U.S. Fire Administration.
- Up to 306 cases of infant abductions took place between 1983 and 2016, most often in health care facilities.
- In 2016, more than 209,000 individuals suffered a cardiac arrest, triggering a Code Blue, in hospitals.
Depending on each facility’s size and level of care, code designations may vary. Among Joint Commission-certified hospitals, most codes maintain industry-wide designations and similarities. However, it is important to check with your local facility administrator or nurse educator for code designations at the time of hiring, re-evaluation, and continuing education. In the interim, you can use this guide as a refresher of common code designations and proper protocols for responding to emergencies in the health care facility.
Insights on Emergency Hospital Codes
Emergency hospital codes help facility personnel understand how to effectively manage emergencies. Depending on the type of facility, emergency codes may be created by internal administrative officials or oversight agencies.
For example, the Department of Aging and Disability Services (DADS) manages emergency code support among home and community support services agencies (HCSSAs) in Texas, like skilled nursing facilities and long-term rehabilitation facilities. In addition, the Centers for Medicare & Medicaid Services (CMS) provides additional direction for all provider types responding to emergencies, particularly those involving community-based or facility-based emergency communication. Training on such emergencies must be conducted at a minimum of every 12 months.
Furthermore, health care facilities only have until November 15, 2017, to draft and finalize emergency preparedness administrative plans for responding to emergencies under new CMS protocols, health care professionals must understand the primary emergency hospital codes first.
Health care professionals trained in ACLS, BLS, PALS, and CPR are better equipped to act swiftly and decisively during emergencies. These courses provide the foundation for managing crises like Code Blue (cardiac arrest) or Code Pink (pediatric emergencies).

Code Designations
Code Grey or Silver – Active Shooter
 An active shooter is defined as an event in which an individual or group Breakdown of Active Shooter Prevalence. Depending on facility preference, Code Silver or Code Grey in a hospital may be used interchangeably. However, Joint Commission standards were updated in 2010, which advise facility managers to use Code Grey to denote active shooter incidents.
An active shooter is defined as an event in which an individual or group Breakdown of Active Shooter Prevalence. Depending on facility preference, Code Silver or Code Grey in a hospital may be used interchangeably. However, Joint Commission standards were updated in 2010, which advise facility managers to use Code Grey to denote active shooter incidents.
During this emergency preparedness code activation, an overhead announcement may be made.
For example, “Security Alert, Active Shooter, South 5, White Male in Blue Jeans.”
However, some hospitals or facilities, to prevent an active shooter incident from worsening, may have taken an alternative approach, not using a code and using plain language only. This may prevent panic and unnecessary loss of life when such an incident occurs. In addition, an announcement may be made to security personnel and supervisory personnel via phone, eliminating panic and giving everyone time to evacuate or shelter in place.
Steps to Follow During a Code Grey
If an active shooter incident occurs, follow these steps:
- Take shelter.
- If a landline phone is available, dial the facility’s active shooter code. For example, Florida health care facilities can activate this code by dialing “20” from a landline phone.
- Give the call center or emergency team on the other end of the line with information about the shooter’s appearance, hostages, location and communications. ONLY DO THIS IF IT IS SAFE FOR YOU TO SPEAK WITHOUT THE SHOOTER HEARING OR SEEING YOU.
- LEAVE THE PHONE “OFF THE HOOK” TO ALLOW RECORDING OF ALL EVENTS TAKING PLACE.
- If sheltering, stay in place until instructed to leave by law enforcement or if the situation permits.
- If the situation is located in another part of the facility, activate all security doors to your unit.
- If security doors are unavailable, barricade the unit with whatever items are available to prevent entry into your unit.
- When hiding and evacuating are not possible, and If your life is in imminent danger, try to disrupt and/ or incapacitate the shooter by acting aggressively, throwing things at him, yelling or by taking other extreme measures.
- It is important to remember your duties to protect the lives of those you serve during this incident.
- When leaving the facility or upon being located by law enforcement, make sure your hands are up and away from your pockets and clearly visible.
Following a Code Grey asserts the Department of Homeland Security (DHS), your supervisor may require all staff members to complete an incident report. This may be required even for floors or units where sheltering in place was used and no loss of life occurred. Such reports can help managerial staff learn from the incident and prepare for the possibility of a future attack.
Code Orange – Assistance Needed or Hazardous Spill
 Code Orange is another code that may have facility-specific meanings. Joint Commission standards define Code Orange as an exposure to a hazardous material or substance within a facility. However, it may be used to denote “attention needed” for violent patient situations or other emergencies. The key lies in understanding a Code Orange’s differentiation from Code Grey. A Code Orange may be called if a patient is being violent during a medical procedure, attempts to leave the facility while under an order of protective custody or another event.
Code Orange is another code that may have facility-specific meanings. Joint Commission standards define Code Orange as an exposure to a hazardous material or substance within a facility. However, it may be used to denote “attention needed” for violent patient situations or other emergencies. The key lies in understanding a Code Orange’s differentiation from Code Grey. A Code Orange may be called if a patient is being violent during a medical procedure, attempts to leave the facility while under an order of protective custody or another event.
Announcements During Code Orange
 Upon activation, an announcement may be made.
Upon activation, an announcement may be made.
For example, “Code Orange, Medical Spill and Location.” Alternatively, “Code Orange, Violent Patient, and Location.”
Depending on your facility’s emergency preparedness plans, the first example may follow decontamination protocols, including mobile showers, hazmat suits or evacuations if necessary.
The second example may have specific guidelines, such as the following:
- Upon activation, all proper, trained personnel may be called to the location of the violent patient. Depending on the facility, proper personnel may include those with training in handling aggressive patients, like Satori Alternatives to Managing Aggression.
- Discuss the specific needs and issues occurring during the event.
- Use communication-based aggression-management techniques to resolve the situation.
- If a court order exists, nursing personnel may be required to forcibly administer intravenous medications, apply restraints or take other specific actions.
- Complete an incident report upon the event’s end.
- Follow up with your supervisor regarding your actions during the event, including reviewing proper protocols and best practices for responding to such events in the future.
Code Red – Fire
 A Code Red denotes the presence or reasonable presumption a fire is occurring in a facility. For instance, a staff member who sees or smells smoke may activate fire codes. In most hospitals or facilities, automatic fire detection systems may alert staff members first. An overhead code may be called as well.
A Code Red denotes the presence or reasonable presumption a fire is occurring in a facility. For instance, a staff member who sees or smells smoke may activate fire codes. In most hospitals or facilities, automatic fire detection systems may alert staff members first. An overhead code may be called as well.
For example, “Code Red, Medical ICU.”
The code may also provide additional directions when appropriate, like “Evacuations underway in Medical ICU.” Some hospitals may also provide additional evacuation codes when calling the code. “Code Red, Medical ICU. Code White Medical ICU.” (Code White will be discussed in further detail later in this article.)
How to Respond to a Code Red in a Hospital
 There are four steps to responding to a Code Red in a healthcare facility, given the acronym, RACE, which include the following:
There are four steps to responding to a Code Red in a healthcare facility, given the acronym, RACE, which include the following:
- Rescue – Rescue all individuals, including staff, patients or visitors, nearest the fire. Do not get belongings, and only bring essential items. For example, a person on life-sustaining IVs or machinery may be moved with patients. Do not worry about non-life-sustaining items or equipment.
- Alarm – Activate the fire alarm if a code has not yet been called. Upon activation, some announcements may be automatic. If an announcement is not made, have a staff member dial the overhead operator or make the announcement, depending on your facility’s protocols. Smaller hospitals may allow any staff member to make overhead announcements.
- Confine – Attempt to confine the fire by closing doors between you and the fire. This will also help prevent the fire from growing. Additionally, avoid moving between fire-barrier doors and areas unless absolutely necessary. Touch the door prior to entering the facility to ensure you are not walking into an inferno.
- Extinguish – Using an appropriate fire extinguisher, attempt to extinguish the fire.
Fire extinguishers also have an acronym for remembering how to use the device and effectively put out the fire, explains the Occupational Safety and Health Administration, PASS:
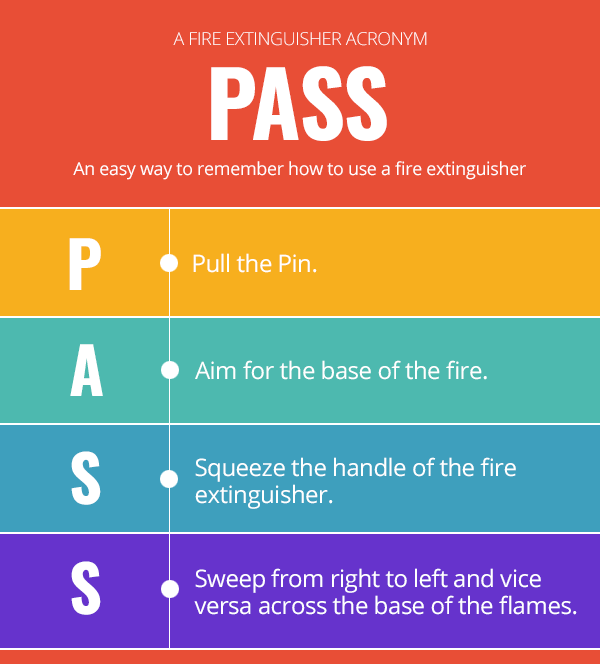
If flames reignite, repeat the process starting with aiming for the base.
In health care facilities, each floor may assign one staff member to go help fight a fire. This staff member should take a fire extinguisher to the unit affected. Do not begin using the “PASS” protocol until arriving at the location of the fire.
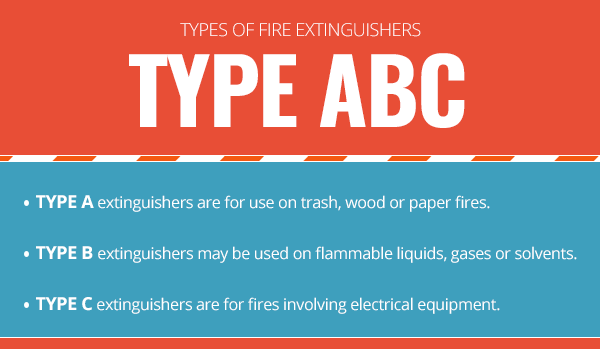
Another factor to consider is the type of fire extinguisher. Some fire extinguishers may be classified as a Type A, B or C. Many modern extinguishers may have a Type ABC, allowing for use on any type of fire.
Provide all necessary medical or emergency care to those injured during a Code Red. This may include staff, patients and visitors alike.
While a Code Red often focuses on fire safety, having certifications like BLS and CPR can be vital for addressing respiratory complications or injuries caused during an evacuation.
Code Brown – Severe Weather
 Believe it or not, a Code Brown is not widely used in health care facilities regarding bowel movements. Although, some hospitals may use “Code Brown” as a non-emergent indicator of bowel movements.
Believe it or not, a Code Brown is not widely used in health care facilities regarding bowel movements. Although, some hospitals may use “Code Brown” as a non-emergent indicator of bowel movements.
Most facilities use “Code Brown” to denote severe weather impacting the facility. Severe weather is defined by any weather event in which reasonable damage and possible injury if exposed to the storm could occur. In other words, storms with golf ball-sized hail, winds in excess of 60 mph, tornadoes and severe lighting are considered indicators of severe storms. Additionally, torrential rain and flooding may call for alerts under this emergency code.
Stages to Follow During a Code Brown in a Hospital
Depending on the size and location of your facility, different protocols may exist for responding to a Code Brown. Each stage reflects the storm’s perceived level of severity and protocols to prevent injury.
Stage 1:
This is the simplest and less-intense stage of severe weather. It may be issued when a severe weather watch is in effect for the area. Any type of severe storm watch, such as a tornado or severe weather watch, may trigger this level of code. Upon activation, there may not be any recommended protocol besides remaining vigilant over possible storm development and organization. However, if you can see lighting or other signs of severe weather from patient rooms, it is best to go ahead and close shades, blinds or curtains.
Stage 2:
The second stage is used when a severe weather warning has been issued. All blinds, curtains, shutters or shades should be drawn. This helps prevent glass or flying debris from entering and harming a patient. Avoid having patients bath during this time as the situation could grow more dangerous suddenly.
Stage 3:
The third stage is the most severe weather code used in health care. It denotes an imminent threat to the facility from severe weather, like a tornado or hurricane-force winds in Tornado Alley. Stop what you are doing, and pay attention to the details of the severe weather announcement.
A typical announcement for Stage 3 may go beyond standard announcements, advising of expected damage location and event. For example, “Code Brown, Stage 3, South.”
In this case, you will need to prepare patients and visitors for the event. Ask all ambulatory patients to leave areas that will be impacted and go to a safe, glass-free location, like the stairwell or interior patient rooms.
Patients in beds that cannot be removed will need to have the bed’s position changed to have the head of the bed raised to its highest position and point the foot of the bed away from the windows. This will provide a shield against flying debris if the windows break. Give patients, visitors, and other staff members items, like blankets, pillows or books to help guard their faces and heads against possible debris.
There may be severe weather events that require a greater response, including evacuation and relocation to a safer facility before and after a major weather event occurs.
Remember to protect yourself if a tornado or other major event directly hits your facility using the tips and advice in this section.
If evacuation is necessary, follow the protocols and steps set forth under “Code White.”
Code Pink / Code Purple– Missing Child
 Code Pink denotes a missing child in health care facilities. However, Code Purple may be used in conjunction with Code Pink to provide additional direction and information regarding an abduction.
Code Pink denotes a missing child in health care facilities. However, Code Purple may be used in conjunction with Code Pink to provide additional direction and information regarding an abduction.
For instance, Code Pink may be used for infants up to six months of age, and Code Purple for all children older than six months.
A standard announcement for Code Pink should include the child’s age, location and other key characteristics.
“Code Pink, 4-month-old infant, Neonatal ICU, Last Seen With a Female Wearing Green Scrub Pants.”
The description should be detailed enough to give most employees, visitors and even other patients the primary means of identifying a person in the facility.
Many hospitals have implemented strict protocols for preventing infant or child abductions, including limiting access to units where children are located, using electronic ankle and wrist monitors for children’s whereabouts and electronic, employee-activated entryways.
What to do during a Code Pink in the Hospital?
If a “Code Pink” is activated, follow these steps:
- Recognize that the individual is statistically more likely to be a female of childbearing age and possibly overweight, reports the Hospital Association of Southern California.
- Check all assigned patient rooms, staff areas and hallways of your unit for the suspected abductor and child.
- Require anyone matching the description to please remove oversized clothing, like heavy jackets to check for the missing child.
- In addition, notify security of any person matching the description prior to confronting the individual.
- Use any means necessary, without putting yourself or the presumed person of interest at risk for violence or injury, to prevent the individual from leaving the facility.
- Call for help if an individual is actively trying to leave a facility with a child during a Code Pink.
- All external doors should be locked upon activation of a Code Pink, and no one should be allowed to leave the facility.
- After locating the child and removing the child from the abductor’s custody, follow up with your supervisor regarding ways to improve protocols and practices if a future event were to occur.
- Only allow individuals to leave the facility upon clearing the Code Pink.
Other Prevention Strategies During Code Pink:
There are a few other ways to help prevent a Code Pink, which include the following:
- Make sure you know who is on the floor. When parents or family members visit children or infants, request photo identification to prevent unauthorized entry to the unit.
- Check all children and parents for proper documentation and safety equipment, like patient-parent matching armbands or electronic monitors, to prevent an abductor from taking a child.
- Report any malfunction of child-safety equipment, especially problems with abduction locks and monitors, at once.
- Report any suspicious behavior to security or appropriate personnel. This tip may be most used when parents have disagreements or court orders limiting contact with children. In some cases, a child’s own parents may attempt an abduction if a court order has removed custody from the parents.
- Teach parents about proper procedures for preventing an abduction. While this may seem irrelevant, parents and guardians may be the most likely to identify a suspicious person, behavior or incident before staff members activate a Code Pink.
Incidents involving child abduction may worsen in hostage situations or incidents involving an active shooter. Follow your facility’s policies and procedures for addressing each code in tandem.
Code Black – Bomb Threat
 A Code Black denotes a bomb threat to the hospital/facility. This may include the identification of an actual bomb within the facility. To prevent confusion, always consider any Code Black to be a verified threat to the facility.
A Code Black denotes a bomb threat to the hospital/facility. This may include the identification of an actual bomb within the facility. To prevent confusion, always consider any Code Black to be a verified threat to the facility.
If a threat is phoned to the facility, try to get as much information about the caller as possible. If the phone has a record function, activate it without notifying the other party on the line. Ask questions about the threat, and signal the issue to other employees to activate the Code.
Try to keep the caller on the line for as long as possible. Ask these questions:
- Where is the bomb located?
- How soon will it detonate?
- Why has a bomb been placed in the facility?
- How do you know a bomb is there?
- When was it placed?
- What do you want in exchange?
- What is your name?
- Do you have a contact number to call you back on?
- Can you tell me anything else about the bomb?
It is important that you remain calm and not get angry at the individual phoning in a threat. Upon the arrival of security or law enforcement, turn the call over to them.
Depending on your facility, an overhead announcement will be made.
“Code Black, Phoned Threat, South 8.” Alternatively, “Security Alert, Phoned Threat, South 8.”
For additional guidance, the DHS Office for Bombing Prevention and the FBI have created a checklist for determining the credibility of a bomb threat.
Determining the Credibility of a Bomb Threat
 A low-risk threat has the following characteristics:
A low-risk threat has the following characteristics:
- The threat is vague.
- Information is inconsistent, lackluster in detail or implausible.
- The caller is easily identified and has made multiple calls.
- The threat was discovered, like finding a package, not receiving an actual threat.
Medium-risk threats may have the following characteristics:
- A direct threat is feasible.
- Wording that indicates the perpetrator has a possible plan for the bomb or threat.
- Indications of a time and place for the bomb to detonate.
- A lack of strong indicators that the person has taken preparation steps for completing the treat.
- Indications of the bomb’s composition.
- The increased emotional state of the perpetrator, like saying, “I’m serious,” or “I’m going to do this.”
High-risk threats are very specific and realistic. The perpetrator may give names, reasons for why he or she is doing this, information about plans to detonate the bomb, including actions taken to ensure its completion, like taking a hostage or using weapons to protect the bomb. In addition, the perpetrator may provide his or her own identity.
Some medium-risk threats and all high-risk situations require immediate intervention. If law enforcement and security professionals have arrived, follow their commands. Otherwise, you need to activate the code denoting an evacuation due to a bomb threat. In this case, the overhead announcement may include a double-code for both a bomb threat and evacuation (Code White), depending on your facility’s protocols. Furthermore, the areas being evacuated should be listed.
“Code Black, Code White, All Personnel in the South Tower.”
How to Respond to a Code Black
Follow these steps in the interim:
- Remove yourself and any individuals in imminent danger from a suspected bomb or package. This includes evacuating the floor or unit if the bomb is located in your unit.
- Contact authorities as soon as possible, and active the Code Black.
- Depending on your facility and the care-level required of your patients, you may need to begin evacuation procedures.
- Unlike Code Grey, do not shelter in place. Begin evacuating the facility, starting with a reverse-triage protocol. (More on reverse-triage protocols will be discussed under “Code White.”)
- If the threat not found to be credible by law enforcement, an evacuation order may be rescinded.
- Law enforcement personnel or administration are usually the individuals ordering an evacuation.
Code White – Hospital Evacuation
 Code White denotes a mandatory hospital evacuation. However, it may not necessarily require a hospital-wide evacuation. In other words, specific floors and areas may be evacuated to improve safety and address the emergency. The announcement may be as follows:
Code White denotes a mandatory hospital evacuation. However, it may not necessarily require a hospital-wide evacuation. In other words, specific floors and areas may be evacuated to improve safety and address the emergency. The announcement may be as follows:
“Code White, Medical ICU.” Since a Code White typically involves another emergency in the facility, additional hospital codes will be called to indicate the reason for the evacuation, assuming an existing code has not yet been activated.
“Code White, Code Red Medical ICU.” If a previous code has been called, like a Code Grey, the overhead announcement will not likely contain a repeat of the Code Grey. The key to understanding how to respond to an evacuation lies in listening carefully to the announcements.
When an evacuation code is activated, you will need to remove as many patients as possible, including their family members, from the affected areas. While you may want to save as many lives as possible, it is important to consider your own safety too. Do not put yourself in a life-threatening situation unless absolutely necessary.
How to Follow Reverse-Triage Protocol during Code White?
To evacuate patients, follow a “Reverse-Triage Protocol.” This protocol is named because unlike triage, you want to move the least-intensive patients first. A standard Reverse-Triage Protocol is as follows:
- Evacuate ambulatory patients.
- Remove wheelchair-bound patients.
- Remove bed-bound patients. If elevators are not function, like during a “Code Red,” drag the patient’s bed with the patient still in bed down the stairs. However, be as careful as possible for patients that have recently undergone surgery or major medical procedures.
- Patients in the middle of medical procedures should be moved as soon as it is reasonably safe to do so. If the procedure is wound dressing or other minor procedure, stop, cover the wound and begin respective evacuation protocols.
- If patient family members are present, ask them to please help with getting their loved ones out of the facility.
Code Green – Emergency Operations Plan Activation
 A Code Green is another emergency code used in health care facilities to denote the activation of the emergency operations plan. This plan may comprise any of the aforementioned hospital codes and the facility’s immediate command centers. Furthermore, a Code Green may be used explicitly for denoting an external emergency in the community or area, like a terrorist attack or a mass shooting.
A Code Green is another emergency code used in health care facilities to denote the activation of the emergency operations plan. This plan may comprise any of the aforementioned hospital codes and the facility’s immediate command centers. Furthermore, a Code Green may be used explicitly for denoting an external emergency in the community or area, like a terrorist attack or a mass shooting.
The processes and steps to respond to a Code Green tend to involve multiple protocols across all hospital emergency. In addition, new CMS guidelines have been released providing additional direction on why Emergency Operations Plan Activation is necessary and how hospitals must prepare for these events.
As a nurse or other immediate caregiver, your facility will provide additional direction on what you need to accomplish and complete with respect to training for new changes in plan activation. Due to the intensive, administrative-driven protocols that must be reviewed and managed in creating an Emergency Operations Plan, the next journal will focus on an in-depth discussion of Code Green and Emergency Preparedness and Operations Planning.
In the interim, follow the commands given by your facility managers and administrators when activating a Code Green.
Code Blue – Cardiac Arrest or Medical Emergency
 Code Blue in a hospital is among the most easily recognized emergency hospital codes in existence. While most associate it with the cardiac arrest of a patient, it may be used to denote any medical emergency in a health care facility, including medical emergencies involving patient family members.
Code Blue in a hospital is among the most easily recognized emergency hospital codes in existence. While most associate it with the cardiac arrest of a patient, it may be used to denote any medical emergency in a health care facility, including medical emergencies involving patient family members.
Upon activation of a Code Blue, listen to the announcement for location.
 “Code Blue, South 6.”
“Code Blue, South 6.”
Depending on your facility, all available staff members from floors adjacent to the affected floor may be called to assist with the code.
Your immediate actions if a code occurs on your floor should be assigned upon reporting for duty.
For example, the Charge Nurse may assign individual staff members to perform compressions, manage airway, document, activate overhead announcements, draw labs and give medications.
If you do not have an assignment for hospital emergency codes at the start of a shift, ask the Charge Nurse about it. He or she may have forgotten to create assignments for a code. In addition, your facility may have an “anyone jump in” policy. This means that the first person to get to the scene will begin with CPR, and all subsequent individuals will “jump in” to help.
It is also important to ensure you have the appropriate credentials for responding during a Code Blue. This may include Advanced Cardiac Life Support (ACLS), Pediatric Advanced Life Support (PALS), Basic Life Support (BLS) and CPR & First Aid training. Training for each type of emergency certification is typically good for two years. However, your individual state or facility may have additional guidelines for completing training more often. For example, nurses in critical-care facilities may be needed to renew certifications annually or complete continuing educational units throughout the year.
Preparing for Hospital Emergency Codes
Every hospital emergency code used is only as effective as the staff members’ understanding of their proper response and responsibilities when a code is activated. If you need any direction on these hospital codes, ask for a supervisor for additional information and training materials. Ensure your ACLS, BLS, PALS, and CPR certifications are current, as they are fundamental to handling emergencies effectively.
Stay prepared for hospital emergencies—get certified or recertified in ACLS, PALS, BLS, and CPR today!
Know what to do if an emergency code is called in your facility, and update your training if any certification will be expiring within the next three months. By taking action today, you can be ready for the emergencies that tomorrow’s day in the life of a health care professional will bring.
References:
- https://news.brown.edu/articles/2015/02/shooters
- https://hhs.texas.gov/doing-business-hhs/provider-portals/long-term-care-providers/home-community-support-services-agencies-hcssa/hcssa-emergency-preparedness
- https://www.cms.gov/medicare/provider-enrollment-and-certification/surveycertemergprep/emergency-prep-rule.html
- https://c.ymcdn.com/sites/www.lhaonline.org/resource/resmgr/imported/Code%20Silver%20for%20website.pdfhttps://www.dhs.gov/xlibrary/assets/active_shooter_booklet.pdf
- https://www.osha.gov/SLTC/etools/evacuation/portable_use.html
- https://www.hasc.org/sites/main/files/file-attachments/2009_emergency_codes.pdf
- https://preparedness.utexas.edu/OBP_BombThreatGuidance.pdf






hi thanks for the info