As a professional directly responsible for patient care, you’re the first line of defense for patients have their worst day possible. You can save a life.
Yet, with all of your advanced medical training, there is one highly complex situation that may give you pause. That hesitation could cause a delay when seconds matter. That condition is hemodynamic instability.
For this reason, I’ve created this complete guide. Whether you’re a paramedic facing another unpredictable, high-stress day or a tech-enthusiastic, patient-care prioritizing nurse, I want you to feel confident that you know how to identify this condition and what to do next.
What is Hemodynamic Instability?
Hemodynamic instability is abnormal or unstable blood flow. Put simply, the body’s circulatory system cannot maintain adequate blood pressure. This deprives the organs of the oxygen and nutrients they need to function—and survive.
This abnormality can quickly lead to dangerously low levels of oxygen reaching vital organs. As the condition progresses, it puts your patient at risk of organ failure. Your patient could experience irreparable injury to critical body systems.
Given the serious damage potential—that may even become fatal—your quick action is paramount. You must manage it quickly and effectively.What’s more, this instability can cause a number of underlying conditions to worsen in a cascade effect.
In your field, recognizing and understanding the signs of hemodynamic instability is crucial for ensuring the best possible outcomes for your patients. If you take the right actions next, you can stabilize your patient. It’s important to stay current with your advanced medical certifications to help you do that.
Before I proceed, and this article gets technical, I want to remind you that this guide isn’t just about how to save a life. The faster you stabilize the patient, the more likely they are to fully recover and potentially go on to live a quality life. That means doing what they love with the people they care about. The work you do every day makes that possible for many.
What Causes it?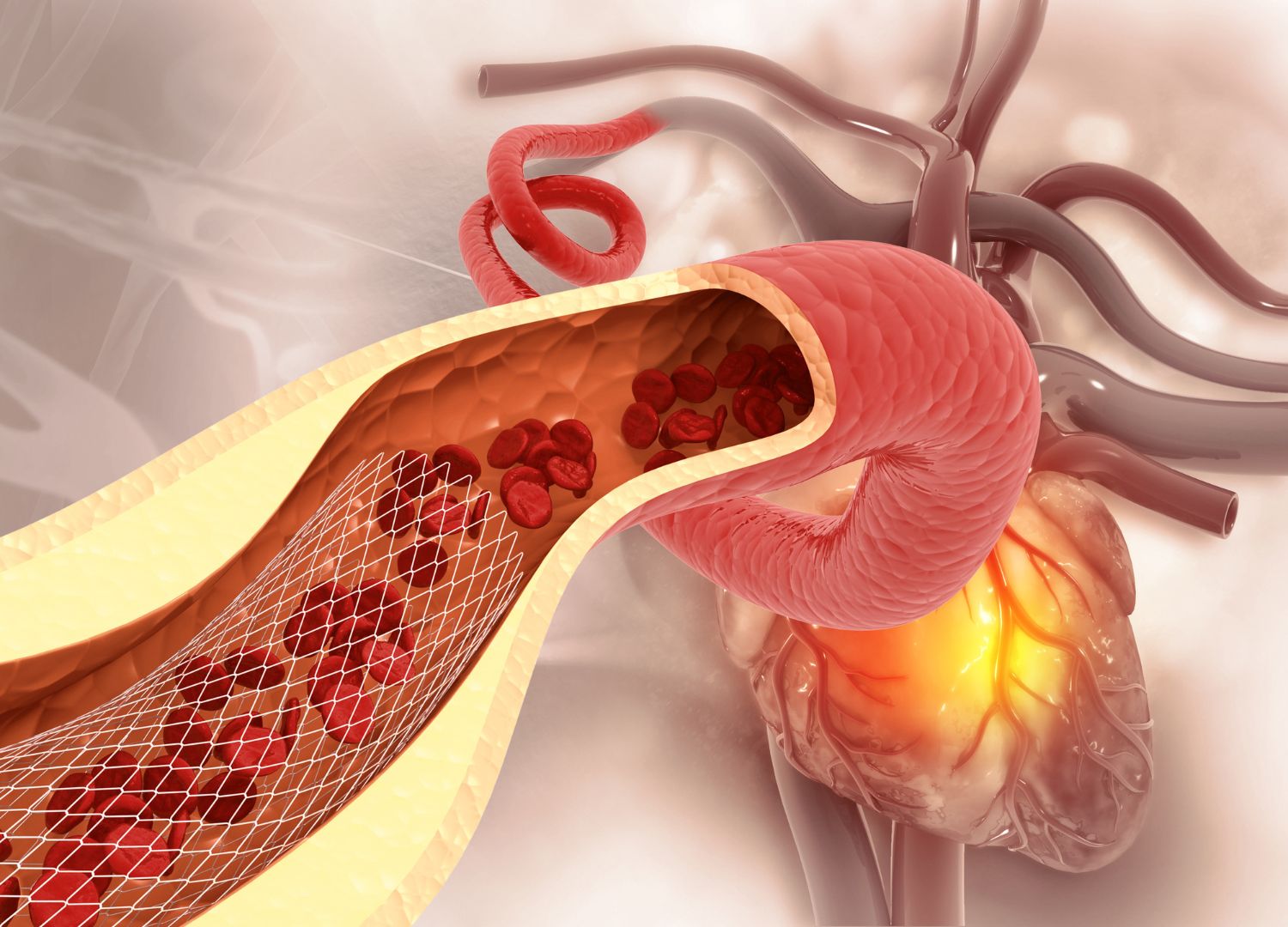
As a nurse, in particular, you are often with the patient before things turn for the worse. Your keen eye on the patient may help your medical team identify high-risk patients. Plus, because you know the patient, you may see signs of worsening hemodynamics before the doctors in the room become aware of it.
If you’re an EMS professional, know that patients can slide into this condition, and the faster you recognize it, the more likely you are to turn the situation around.
Identifying this condition begins with understanding the cause that can lead to these dangerous blood pressure fluctuations.
1. Trauma
Severe physical injuries can lead to external blood loss or internal bleeding in your patient. If the loss is significant, changes in hemodynamics are not just a possibility; they’re inevitable. Your patient’s circulatory system is compromised. It no longer has control over how much the heart can pump.
Now, it can’t maintain adequate blood pressure and perfusion (blood flow), no matter how hard the heart works. As the heart tries to compensate by beating harder and faster, it can quickly wear itself out.
2. Cardiac Events
Certain heart conditions can impair your patient’s ability to pump blood effectively, leading to instability.
These include but aren’t limited to:
- Myocardial infarction (heart attack)
- Arrhythmias (abnormal heartbeat timing)
- Cardiac tamponade (fluid accumulation in the pericardial sacs, compressing the heart)
3. Sepsis
When a severe infection spreads throughout your patient’s body, the immune system reacts. In some cases, overreacts. Rampant inflammation results.
This leads to vasodilation (widening of blood vessels) and reduced blood pressure. In fact, these two are so connected that septic shock is considered a type of hemodynamic instability.
4. Hypovolemia
This occurs when your patient loses significant fluids and doesn’t have enough water to restore proper function. Some common culprits include:
- Severe dehydration
- Hemorrhage
- Burns
5. Pulmonary Embolism
During this blockage in one of the pulmonary arteries in the lungs, your patient can experience a sudden drop in blood flow. This escalates to changes in hemodynamics and respiratory distress.
Without enough liquid volume in the circulatory system, your patient struggles to maintain blood pressure. Understanding the causes can also help you determine if your patient is experiencing this. You can make more informed decisions about what to do next.
How to Determine Hemodynamic Instability
You have several key technologies at your disposal to quickly identify and monitor this condition. Those tools may vary a little depending on your role as an EMS professional in the field, a home caregiver with monitoring equipment, or a nurse checking in on their patients. However, the things to look for remain the same.
1. Blood Pressure Measurement
This one sounds like a no-brainer, but hear me out. During an emergency, even the best of us can overlook obvious signs because we’re hyper-focused on certain symptoms, ignoring others.
One of the first indicators of hemodynamic instability is abnormal blood pressure—you already know that. However, it would be a mistake to ONLY look for low blood pressure. That’s because both hypotension (low blood pressure) and hypertension (high blood pressure) can be signs that your patient is struggling to maintain adequate circulation at different stages of the situation.
2. Heart Rate Monitoring
Similarly, both tachycardia (a rapid heart rate) or bradycardia (a slow heart rate) can signal that the cardiovascular system is under stress. Your patient’s irregular heartbeat might also indicate a more serious underlying issue contributing to instability.
3. Capillary Refill Time
Delayed capillary refill time (longer than 2 seconds) can suggest poor blood flow. This sign is more likely if your patient is going into shock.
4. Mental Status
Is your patient acting confused, agitated, or unresponsive? Each of these altered mental statuses can tell you the brain isn’t receiving enough oxygen. This would be a direct result of inadequate blood flow.
5. Skin and Body Signs
Look at your patient’s face, arms, and legs. Do you see pallor or cyanosis (bluish skin)? You might also notice diaphoresis (excessive sweating). These can be outward signs that the body is distressed. Your patient may also have cold hands, arms, legs, or feet as well as decreased urine output.
6. Rapid Breathing (Tachypnea)
If your patient is experiencing blood loss, then you may notice this sign in conjunction with an elevated or irregular heart rate. As they lose fluids, the heart rate goes up.
They may start to breathe faster as the lungs try to maximize the oxygen in what little blood the heart can pump. After a time, however, the breathing starts to slow (bradypnea). This could be confused with a sign that they’re stabilizing. However, it more often means the opposite. The lungs are taxed, and respiratory failure is imminent.
How to Treat Hemodynamic Instability in EMS
Treating this condition is a race against time. You don’t have access to a whole hospital’s worth of medical technology and equipment.
Your primary goal is to stabilize your patient’s condition to increase their chances of survival on their way to the hospital. It helps to think about it in seven steps, which will, of course, overlap with your typical EMS protocols (usmle.org, NAEMT.org). Please review your training before attempting, as these are high-level summaries that cannot replace your training.
1. Initial Assessment and Rapid Identification
Before any treatment can begin, it’s crucial to perform a rapid but thorough assessment. Identify the signs of hemodynamic instability above. See if you can identify the causes. Use your assessment skills to prioritize interventions.
Take a look at this FREE Advanced Cardiac Life Support Course from Save a Life for more details.
2. Airway, Breathing, and Circulation (ABCs)
Next comes the foundation of emergency care, which you know by heart.
- Airway: Ensure the patient’s airway is open and protected. Is your patient unresponsive? Consider airway adjuncts like an oropharyngeal airway (OPA) or a nasopharyngeal airway (NPA). If you have identified significant instability, begin advanced airway management, such as intubation (trachea tube).
- Breathing: Assess the patient’s respiratory rate, effort, and oxygen saturation. It may be time to administer high-flow oxygen or assist with ventilation. If your patient experiences respiratory distress or oxygen levels below 90%, think about using positive-pressure ventilation.
- Circulation: Establish IV or IO (bone marrow) access ASAP. Start giving your patient fluids like normal saline to help raise blood pressure and improve circulation. If the fluids alone aren’t enough, consider using medications to help maintain blood pressure.
3. Control Hemorrhage (if trauma)
Is the patient’s instability caused by trauma with significant bleeding? Then, your next course of action is to control the loss fast. Apply direct pressure and tourniquets for limb injuries or hemostatic gauze for trunk, head, and face bleeding. Follow Bloodborne pathogen management protocols.
You won’t get far with this patient until you can stop the bleeding to improve circulation. As you do, you begin turning the tides of your patient’s declining situation.
4. Manage Cardiac Events
As you continue hemodynamic monitoring, stay vigilant for cardiac issues that require fast action.
If your patient experiences bradycardia without an obvious reversible cause, start atropine. If the patient doesn’t respond, begin transcutaneous pacing (TCP) to temporarily regulate the patient’s heart.
If your patient experiences tachycardia, synchronized cardioversion may be more appropriate. But that’s only if the rhythm is regular but symptomatic.
For irregular rhythms, such as atrial fibrillation, pharmaceutical intervention might be required.
Don’t forget to study your ACLS algorithms before you get into this kind of situation. They can guide you through decision-making processes like these.
5. Address Other Causes
For sepsis, administer fluids aggressively and consider starting antibiotics.
For anaphylaxis, administer epinephrine immediately, followed by antihistamines and corticosteroids. Continue respiratory support.
For pulmonary embolism, provide high-flow oxygen. Then, prepare for rapid transport to a facility capable of advanced intervention.
6. Hemodynamic Monitoring and Reassessment
At this point, your team has set up ECG monitoring to watch for changes in cardiac rhythm that may require intervention. Continue to monitor your patient’s vital signs, mental status, and skin condition. Frequently review the signs to determine if your treatments are effective. You may need to make adjustments.
A recent study evaluated the Analytic for Hemodynamic Instability (AHI), a noninvasive ECG-based technology, to predict hemodynamic instability without continuous blood pressure measurement. It showed high sensitivity and specificity. This suggests AHI could provide continuous monitoring for early detection of instability in hospitalized patients, potentially improving outcomes and resource allocation. (Nih.gov) I anticipate we’ll see it more in mobile emergency medicine as time goes on.
7. Prepare for Transport
Now that you’ve stabilized your patient as well as possible within your scope of practice, it’s time to get them to the nearest hospital. Continue hemodynamic monitoring and provide care on your way to the facility.
What is Hemodynamic Instability? Do You Know the Answer?
You can learn more about hemodynamic monitoring, managing patients, and saving lives when you complete advanced medical certification courses 100% online through Save a Life. All Save a Life training is jointly provided by the Postgraduate Institute for Medicine (PIM). Save a Life is accredited to provide medical training from continuing medical education credits by the Accreditation Council for Continuing Medical Education (ACCME), the Accreditation Council for Pharmacy Education (ACPE), and the American Nurses Credentialing Center (ANCC).
Are you ready to manage your next life-threatening emergency? Get certified with Save a Life’s ACLS certification.
Frequently Asked Questions about Lack of Hemodynamic Fluctuations
Is low blood pressure an indication of hemodynamic instability?
Yes, low blood pressure often indicates hemodynamic instability. However, look for other signs like changes in mental status and skin color variations to quickly determine what you’re dealing with.
What are the vital signs for hemodynamic monitoring?
Blood pressure, heart rate, respiratory rate, oxygen saturation, capillary refill, and mental status are key vital signs for hemodynamic monitoring.
What is hypoxemia in hemodynamic instability?
Hypoxemia is low oxygen levels in the blood. It’s often seen in hemodynamic instability due to poor circulation or respiratory system issues.
What is anaphylaxis with hemodynamic instability?
First, anaphylaxis is a severe, life-threatening allergic reaction. It causes a rapid and significant drop in blood pressure. This can lead to inadequate blood flow to vital organs.
This condition occurs because your patient is having an extreme immune response to an allergen. This has triggered widespread vasodilation (widening of blood vessels) and fluid leakage, resulting in a drastic drop in blood pressure and unstable hemodynamics.
Your ability to immediately give treatment can save their life. You may need to administer epinephrine, fluids, and other supportive measures to stabilize the patient and prevent organ failure. These actions can restore hemodynamics when anaphylaxis was the primary cause.
Can you do a C-section with hemodynamic instability?
If it’s within your scope of practice, you can perform a C-section when someone has hemodynamic instability. However, immediate and careful stabilization is required to ensure the safety of the mother and fetus.






Leave a Reply