1. 2020 ILCOR Guidelines: Algorithm Updates for Pediatric Systems of Care
The 2020 ILCOR guidelines have arrived, leading to new algorithms and guidance.Save a Life has updated its Pediatric BLS Algorithm to reflect the changes and shares ongoing topics they’re reviewing. What’s changed in the guidelines? And what topics are currently under review in the world of pediatric life-saving care? Read the blog and watch the video below to learn more.
Pediatric BLS Algorithm Changes Due to 2020 ILCOR Guidelines
CPR/Chest Compressions for Infants/Children have changed. While cardiac arrests among children outside the hospital are rare, they are most common among infants and males. According to research published in the NATURE Journal, an overwhelming majority (81%) of cardiac arrest in children is due to respiratory failure. Studies have shown the most common cause of respiratory failure is in this order:
- Sudden infant death syndrome (SIDS) (29%)
- Medical causes such as disease, allergic reaction, etc.(25%)
- Trauma (10%)
- Airway restriction due to blockage, drowning, or intoxication
According to the American Academy of Pediatrics, children who experience out-of-hospital cardiac arrests have around a 26% chance of survival past discharge if they reach the emergency department. Of course, this rate can vary significantly depending on education, access to care, etc.
Improving this survival rate is an ongoing challenge for the medical community to face. And ILCOR is continuing to review research to understand what can be done to improve survival rates. For this reason, they’ve released this update as part of their 2020 ILCOR guidelines.
The Old ILCOR Guideline Vs. New Pediatric BLS Guidelines
The guideline change is related to what defines a palpable pulse and how many rescue breaths should be given. In short, one set of CPR consists of 15 compressions and two breaths.
“The old guideline said if there is a palpable pulse 60/min or greater, but there is inadequate breathing, give rescue breaths at a rate of about 12 to 20/min (1 breath every 3-5 seconds) until spontaneous breathing resumes.”
They’ve revised this to say, ” For infants and children with a pulse but the absence of, or inadequate, respiratory effort, it is reasonable to give 1 breath every 2 to 3 seconds (20-30 breaths/min). ”
In other words, the number of breaths per second has increased, and they eliminated confusing language about the number of beats per minute in favor of “any pulse”. This language change may seem subtle, but it isn’t. In the BLS setting, eliminating instructions to count the pulse before making a decision would increase the time before CPR begins at a time when seconds matter, especially if there is only one rescuer.
The current Pediatric BLS algorithm can be found here.
Other Pediatric Basic Life Support Changes In the Works
ILCOR guidelines are constantly evolving, so we can expect new guidance soon related to Pediatric Basic Life Support and Pediatric Advanced Life Support. Some critical topics currently being reviewed in 2020 for guidance in the coming years include the following.
Review of Fluid Administration Rate for Septic Shock
ILCOR has identified a set of studies that need further systematic review. So we can expect updates on this topic soon.
Initial Dose and Dose Intervals for Adrenaline/Epinephrine In Case Cardiac Arrest
For 50 years, epinephrine has been a cornerstone of resuscitation among children. Important to note that administration should be IV/IO at 3-5 minute intervals not exceeding 1 mg in total dosage.
Even its effectiveness in children has not been objectively reviewed. The group’s initial findings based on the evidence call for the shortening the time to first administration may improve children’s outcomes. But ILCOR plans to dig deeper into available research to provide clearer guidance on that and surrounding administration questions.
How to Manage Traumatic Shock in Infants and Children
While much of the data is purely observational, the task force believes they now have sufficient data to systematically review how traumatic shock is managed in infants. They believe they will provide guidance to help professionals evaluate how much fluid and crystalloids to administer. More on this soon.
Ventilation Rate With Advanced Airway During CPR
In 2010, ILCOR’s PLS task force determined that there was not enough data to determine an ideal ventilation rate for children, so they used the adult rate of breaths. They believe more research is needed, so they are reviewing this and may make changes in the future. But they believe they have enough to increase the breath-give rate as stated in the above mentioned 2020 ILCOR Guidelines Update.
What to Do As Guidance Changes
Doing what’s best for the survival and quality of life of children who experience cardiac arrest will always be a moving target. ILCOR will continue to review newly available data and question old practices that may not be best for the patient. And Save-A-Life will keep updating its charts, algorithms, study guides, and courses to reflect the most up-to-date ILCOR guidance.
You must stay current on ILCOR’s latest guidance as well as the topics they’re continuing to review. And if your PALS certification has lapsed, it may be time for a Pediatric Advanced Life Support Recertification to get you current on everything that’s changed since your last certification.
2. 2020 ILCOR Guidelines: Algorithm Updates for Adult BLS & ACLS Systems of Care
First Aid, BLS, ACLS– the science-based best practices for these may seem set in stone. But they are always changing, as 2020 ILCOR Guidelines Updates will show. New data becomes available, new studies organized, and better collaboration of institutions lead to new insights as well as clarifications. What’s new in 2020 guidance for 2021 and beyond? Check out the highlights for BLS and ACLS.
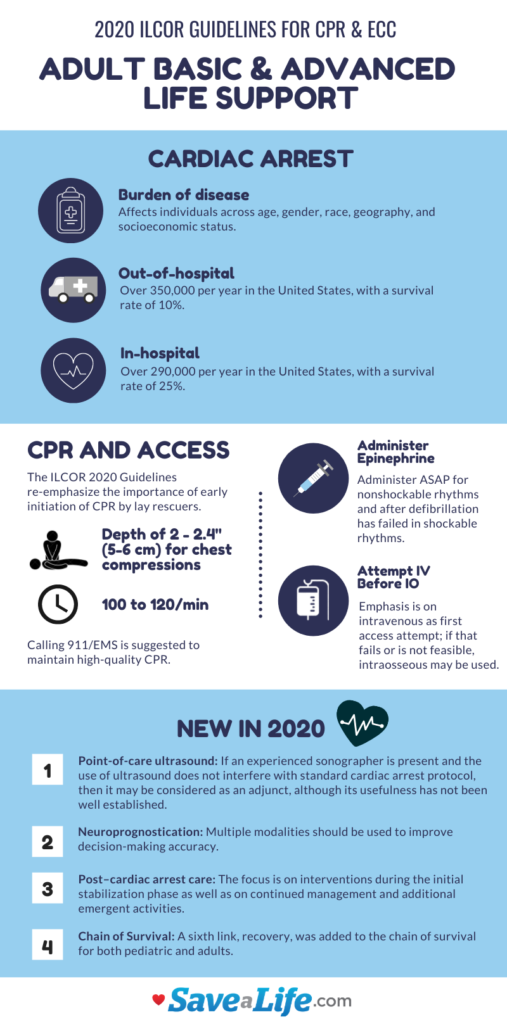
Cardiac Arrest Continues to Be a Concern
Cardiac arrests can affect everyone. Young and old, optimal health and those with chronic disease, every race, every financial group, across geography. There is definite room for improvement, prompting ILCOR to continually review data and refine its guidance.
What’s Changing in BLS & CPR?
Emphasis on Layman CPR
ILCOR 2020 Guidelines re-iterate how important it is to start CPR early. When someone has a cardiac arrest outside the hospital, waiting for EMS to arrive is not an option. Someone needs to start CPR even if they lack confidence because this is their first real-life cardiac arrest, or it’s been a while since their training.
The survival rate of 10% for out-of-hospital events can go up when someone starts CPR. But regardless of a layperson or professionals training, calling 911 is always advisable, as is part of the algorithm.
CPR And Access
The current 2020 guidance calls for a depth of 2-2.4 inches (5-6 cm) for proper chest compression at 100 to 120 compressions per minute. When available, they recommend epinephrine administration immediately if the rhythm is not shockable or if shocking has failed despite a shockable rhythm.
During BLS, they emphasize the importance of attempting intravenous (IV) access to start a drip first before trying Intraosseous (IO) infusion. IO infusion is the preferred route whenever IV access is unavailable, offering a rapid, safe, and effective alternative.
You can see the full Adult BLS algorithm here.
What’s Changing in ACLS with 2020 ILCOR Guidelines?
Point-of-Care Ultrasound
When a sonographer is available, and ultrasound can be performed without interfering with resuscitation efforts, it can be used with other procedures. This is not a recommendation in favor of the ultrasound and rather a statement that it’s okay when it can be done safely. More research is needed to confirm how the ultrasound may improve patient outcomes.
Neuroprognostication
2020 ILCOR guidelines recommend that multiple tests such as those looking for various biomarkers, neurological activity, physiological indicators, and imaging results should be used to verify whether life-sustaining measures should be stopped. They emphasize that no one test can eliminate false positives, especially in a comatose patient.
Post-cardiac Arrest Care
Many people survive a cardiac arrest in the hospital or out of the hospital but do not make it to discharge. ILCOR’s systematic review of comprehensive data has shown that increasing the focus on interventions during the initial stabilization phase and improving how patients are managed after an event can improve a patient’s chance of surviving to discharge and beyond.
Chain of Survival
A sixth link in the chain has been added. So previous guidance includes these five:
- Recognition that a cardiac event is taking place and calling 911
- Activation of the emergency response system
- Immediate high-quality CPR
- Rapid defibrillation
- Advanced live support and post-arrest care
The six links now include:
- Recognition that a cardiac event is taking place and calling 911
- Starting CPR early
- Rapid defibrillation
- Advanced care by Emergency Medical Services
- Post-cardiac Care
- Recovery, including observation, treatment, follow-up care, psychological support, financial support if needed, and rehab
How to Stay Up-to-date with 2020 ILCOR Guidelines and Beyond
The only constant is change. As science advances and organizations like ILCOR.org gather more data, industry best practices will adapt to provide better guidance to everyone, from the average bystander performing CPR to the medical professionals who can provide more advanced care.
While some changes may be subtle, ILCOR is constantly reviewing data, so many things can change in just a few years. For patients’ sake, it’s critical to stay up-to-date so we can all work together to save lives.
Save-A-Life keeps abreast of all the updates and quickly incorporates them into the study guides, courses, infographics, and algorithms that help you stay current. So if it’s been a little while since your recertified in BLS or ACLS, now is a great time to update your certification online and earn continuing education credits through a Joint Commission Compliant organization.[/vc_column_text][vc_column_text]
3. 2020 ILCOR Guidelines: The Latest Updates to First Aid
2020 has been a big year for everyone. But ILCOR has still been hard at work compiling patient and hospital data to better understand what actions can reduce losses and save lives. You may find some of these guidelines already be common practice, but keep in mind these are established on the latest science and help individuals and the medical community advance. There’s a lot to share in the 2020 ILCOR guidelines updates for first aid. Let’s take a look.
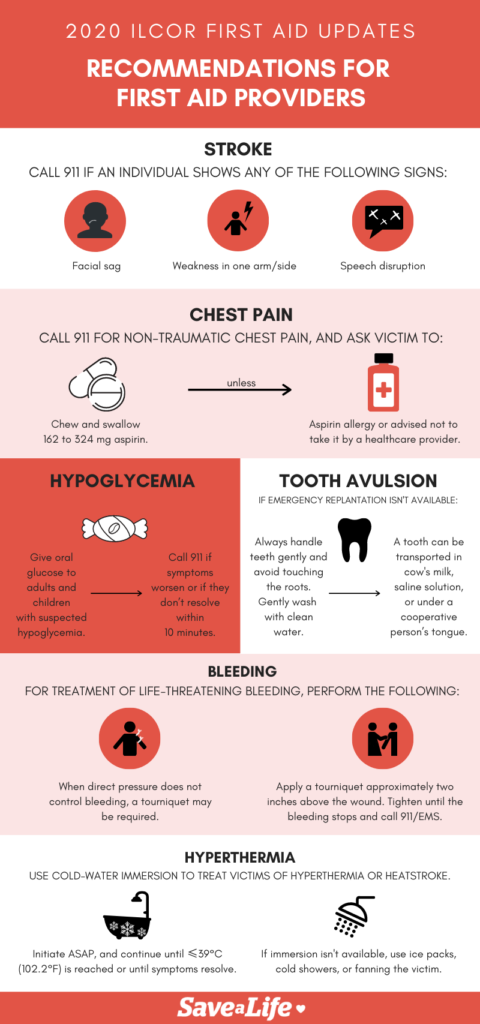
When to Call 911
Some people are quick to call 911 at even the hint of an emergency. Others delay calling because they believe they can help the person without involving EMS. So ILCOR’s 2020 Guidelines outline several cases where it’s ALWAYS an emergency.
Signs of a Stroke
Always call 911 if you notice these serious stroke symptoms.
- Sagging face
- Weakness on one side, especially one arm
- Speak disruptions that may impact how the person speaks or their ability to understand what you’re saying
Due to Chest Pain
Chest pain can have many causes. If a known trauma does not cause it, you should call 911 and have this person checked out to rule out a heart attack. While awaiting emergency services, ask them to chew or swallow an aspirin (162mg to 324mg). That’s 2 to 4 low-dose aspirin. If the person has a known aspirin allergy or has been told not to take aspirin, they should decline and wait for help.
What to Do for Hypoglycemia
If you suspect low blood sugar (hypoglycemia) in a child or adult, usually a diabetic, you should give them oral glucose if they have glucose pills. When glucose pills aren’t available, a small amount of jelly beans, sugar water, candy, jelly, honey, etc. may help. If the person isn’t feeling better in 10 minutes, call 911.
Signs of hypoglycemia include:
- Shakiness
- Sweating
- Hunger
- Fast heart beat
- Inability to concentrate
What to Do for a Tooth Displacement
A tooth avulsion is a tooth displacement, most commonly happens when the tooth is dislodged from its socket. A dislodged tooth can often be reimplanted if care is taken to secure the tooth and you get an emergency visit with your dentist.
Even if emergency dental isn’t available, you may be able to have the tooth re-implanted if you follow some steps.
- Find the displaced tooth
- Don’t touch the roots; this can compromise the integrity of the tooth.
- Wash the tooth with clean water
- Place it in cow’s milk, saline, or under the tongue of the person who lost it to keep it from drying out, as long as there is minimal risk of the person (usually a small child) swallowing it
What to Do When Someone’s Bleeding
If a person is losing blood at a rate that might be life-threatening, take the following steps.
- Apply direct pressure to the site of bleeding.
- If direct pressure is ineffective, apply a tourniquet about 2 inches above the injury. Tourniquets should only be applied to the upper and lower limbs.
- Securely tighten the applied tourniquet until the bleeding stops.
- Call 911
What to Do for Hyperthermia
Hyperthermia is when someone gets dangerously hot, as opposed to hypothermia where someone is too cold. Hyperthermia could occur if someone was unable to get out of a hot car, was exercising in the heat, or spent too much time in a sauna. In extreme cases, heat stroke and loss of consciousness may occur.
Signs of hyperthermia include:
- Nausea
- Fast, strong pulse
- Very weak pulse
- Headache
- Confusion
- Dizziness
2020 ILCOR Guidelines recommend immersing them in cold water. Even if they say they feel better, continue to keep them in cold water until their temperature goes down to 102F, or they feel absolutely fine. Use ice packs, a water hose, a cold shower, and as a last resort, fanning them if putting them in cold water isn’t an option.
First Aid Can Save Lives
When someone experiences an event, often it’s what the bystanders do to save them that makes the difference. Waiting for emergency help can be a deadly mistake. Almost anyone can learn CPR and First Aid. And you can learn it today and get certified online.
Did you find it helpful? Share your feedback with us.







Great post! just infographics are a little blurry and hard to interpret.