AS OF EARLY JULY, the Senate’s work on the AHCA, scored by the Congressional Budget Office (CBO), is expected to result in more than 22 million Americans losing their health insurance. Meanwhile, the number of Americans who could lose insurance in the first year is expected to exceed 15 million, reports Thomas Kaplan and Robert Pear of The New York Times. Yet, the determination of the GOP to pass the bill remains unchanged, regardless of the recess for Independence Day.
 The backlash to the ACA was strong, and the backlash to the current draft of the AHCA is strong. Both the ACA and AHCA want to help people, ranging from the ill to small-business owners. Unfortunately, the impact of the bill could be devastating to the health care industry, especially among health care facilities that provide care to those without insurance, like hospitals and emergency facilities. Rather than discussing the political benefits and cons to the proposed version of the AHCA, your organization needs to understand what the bill’s passage will mean for your future.
The backlash to the ACA was strong, and the backlash to the current draft of the AHCA is strong. Both the ACA and AHCA want to help people, ranging from the ill to small-business owners. Unfortunately, the impact of the bill could be devastating to the health care industry, especially among health care facilities that provide care to those without insurance, like hospitals and emergency facilities. Rather than discussing the political benefits and cons to the proposed version of the AHCA, your organization needs to understand what the bill’s passage will mean for your future.
Key Impacts of the AHCA on Health Care Organizations
1. Decreased Funding Will Drive Overhead Costs Upward
The AHCA revokes the individual mandate within the ACA, implying people do not have a legal or financial reason for obtaining health insurance. This also means fewer people will be enrolled in health insurance across the country. To insurers, it means a return to greater profitability, but for health care facilities, overhead costs will soar, explains Laura Dyrda of Becker’s Hospital Review.
Paying overhead costs depend on the fulfilled financial responsibilities of patients and clients. In other words, hospitals can expect increased payment refusals and additional financial costs in attempting to collect debts from those without insurance. Since fewer people will have health insurance, the risk of seeing patient in extremis, when preventative is insufficient to treat a condition, increases. Therefore, hospitals will face higher treatment costs in the hope of a future payment.
Another issue driving costs upward is Medicare and Medicaid payments. Prior to the ACA, Medicare reimbursement to health facilities was higher. However, the decrease in reimbursement defined by the ACA was created to offset the increased finances coming from insured patients. Yet, the current draft of the AHCA does not restore the pre-ACA reimbursement schedules. As a result, hospitals and health care facilities will continue receiving ACA-dictated reimbursements without the income associated with treating more patients with insurance.
2. Training Programs May Lose Access to Grants and Other Forms of Funding
A key benefit in the ACA was the expansion of Medicaid, including expansion of funds marked for training and research purposes. If the AHCA passes the Senate and its second trip to the House, the current cuts to Medicaid will translate into fewer grants and programs to health organizations. Moreover, the AHCA imposes tax eliminations throughout the economy, which result in less money available for use in state-sponsored or federal programs.
The AHCA also makes it difficult for health care facilities to provide continuity of care. Continuity of care has roots in providing adequate training to all health care professionals. Over time, the current draft of the bill will cut more than $880 billion from Medicaid by creating a capped funding system. In other words, states would no longer receive reimbursement and payments for Medicaid programs based on the severity and per-patient costs associated with providing care.
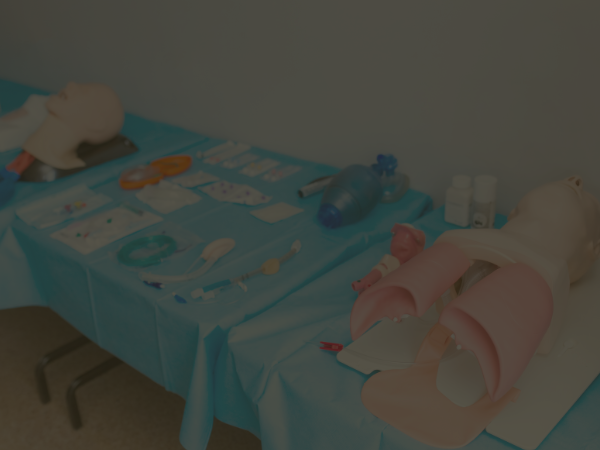
Instead, states would receive a predetermined, per-patient payout for all eligible beneficiaries, reports Lynda Flowers of AARP. Consequently, the per-patient cap will be severely insufficient to cover the rate of increasing health care costs. This will lead to less finances available in facilities for training. Employees may lose access to employer-paid training programs, including required annual training programs, like HIPAA, Bloodborne Pathogens and Basic Life Support and Advanced Cardiac Life Support (BBP, BLS & ACLS).
Simply put, the AHCA’s decreased funding for Medicaid is both unsustainable and life-threatening, especially among emergency care centers. If health care professionals cannot afford to complete training when self-pay or partial self-pay for training programs are necessary, every patient-provider interaction becomes an opportunity for error that could cost someone their life. But, this is not the only way the AHCA will impact health care professionals.
3. Changes in Employer-Offered Health Insurance May Impact Employee Retention
The AHCA will reverse the ACA’s mandate for business owners to offer health insurance. While large organizations, like major hospitals in metropolitan areas, may have offered health insurance to employees prior to the ACA, smaller facilities, like skilled nursing facilities, private practice employees and long-term acute care facilities, may return to pre-ACA benefit levels. In other words, these smaller facilities may not continue offering health insurance to their employees under the new bill.
Health care professionals know the financial costs and burden of health care. So, it is reasonable to assume employees working in facilities that make changes to insurance offerings may consider relocation to an insurance-offering facility. The facility’s existing health care plans and offerings are not limited to the AHCA either. In other words, health care facilities could still offer health plans that fall within the ACA’s guidelines, if health insurers are willing and able to continue offering such plans. Thus, more employees may continue in these facilities, simultaneous with the exodus from smaller health providers or care settings.
4. The Burden of Care Will Shift More Toward Nurses and Direct-Care Staff
Regardless of where health care professionals, including nurses and direct-care staff decide to work, there is another problem with the AHCA. Its treatment-when-severe nature eliminates the funding sources for preventative services and care. As a result, direct caregivers, such as nurses, nursing assistants, home health aides and other caregivers, will face the added pressures of monitoring for issues that could be prevented without the funding of preventative services.
For example, less funding for preventative laboratory work may require nurses to monitor patients’ diets more strictly during inpatient stays. In the outpatient setting, like a doctor’s office, nurses will need to conduct intense assessments looking for any signs of preventable conditions without funding.
In a sense, this is the same duty nurses have always had. They look for what others missed. But, the key difference is funding. More patients paying out-of-pocket will reduce the number of patients authorizing medical screenings or laboratory tests. Consequently, preventative care testing, screening and management of chronic conditions, like diabetes, renal insufficiency or obesity, will become obsolescent, leading to increased health care costs later for patients, family members and health care organizations.
5. Preventative Care Services Will Decrease in Availability
The importance of preventative care services cannot be overstated. Preventative care services are essential to mitigating future health care costs. While certain conditions, like obesity, can be managed through dietary changes and exercise, some conditions requiring preventative care cannot.
For example, early onset diabetes may have a genetic basis, and those diagnosed may need extensive preventative services, including periodic laboratory testing to check bodily systems. But, what else may happen if preventative care services lose funding under the AHCA?
Preventative care relies on a steady stream of incoming patients, seeking to take advantage of preventative care benefits. When those benefits cease to exist, patients turn to hospitals as the insurers of choice, not actual insurance companies. This results in a shift in the number of preventative services available.
Hospitals divert funding from preventative care programs to urgent and emergency care facilities. As more patients wait to obtain health care, due to lack of personal finances or inability to find programs, existing preventative care programs struggle to continue operating. Therefore, the overall number of preventative care facilities and programs decrease, creating a self-fulfilling cycle of decreasing access to preventative care and driving up costs among the last-resort funding sources, such as hospitals.
6. Telehealth Programs May Lose Guaranteed Coverage Status
Applying the internet to increase access to health care, telehealth, was a breakthrough. While most states and the District of Columbia have passed laws to require health insurers cover telehealth services, that fact could be on the chopping block if the AHCA becomes law. Under the ACA, health insurers were obligated to provide coverage to areas without sufficient resources. While this mandate did not expressly cover telehealth services, most insurers interpreted it as such. If the new bill becomes law, this interpretation will change.
The AHCA will act as an opening bell for the backtracking of laws mandating telehealth coverage. However, health insurers have an incentive to continue offering telehealth coverage. It has fewer costs and reduces the overall costs of health care. Ergo, the per-patient costs from providing coverage for telehealth services decreases across an insurer’s membership or covered individuals. But, telehealth programs, especially those using innovative technology and communication tools to distribute services to rural and over-populated areas, need funding from somewhere.
Unfortunately, few statistics exist to support an exact determination on how decreased funding under the AHCA may translate into fewer telehealth resources. In other words, the number of apps and systems created for telehealth purposes may decrease as funding for research and development of these apps decrease. Consequently, existing telehealth system providers and vendors may gain a monopoly over the market, which will inherently decrease competition and lead to spikes in the cost of using telehealth. Thus, insurers may have an added incentive to drop telehealth coverage or at least lobby for reversal of local mandates regarding telehealth coverage.
For patients, health care providers and health insurers, the AHCA may be the first step toward making telehealth unaffordable and unrealistic when compared to the costs of accessing health care elsewhere.
Other Concerns About the AHCA
When Will the AHCA Take Effect if Passed?
There is no way to know exactly when the AHCA will pass, and as a result, it is impossible to narrow down a time of impact. However, the current Congress was unable to achieve its passage prior to 2017’s Independence Day, and thus, it is more difficult to legislators to pass the bill in time for a September 2017 effective date.
Even if the bill were to pass, its scope would require a significant delay to allow health insurers and patients find alternative resources. Moreover, it will undoubtedly face immediate lawsuits at the hands of the nation’s sickest and most vulnerable citizens. Even today’s health insurers have expressed an immense concern over the regulations and statutes within the current draft of the AHCA.
What Do Health Insurers Think About the AHCA?
Think about what sets the standard for health insurance companies; they derive value by paying for services among people who have had continual health insurance coverage and few health problems. This goes back to funding for individuals during periods of monetary crisis, using Medicaid or Medicare to address health problems when obtaining company-based health insurance coverage was not possible. Prior to the ACA, people used Medicaid and Medicare when necessary to treat problems as they came, but the AHCA does not have any mandates for covering pre-existing conditions, and the deficit in Medicaid funding could leave insurance providers on the proverbial hook.
If a person forgoes health care long enough, it can lead to serious health problems. But, if a person simply avoids the issue for the right amount of time, he or she may obtain health coverage through a company under the AHCA, not having previously had any reported problems. Now, the person’s use of health care increases, but the soaring costs of health care, due to the AHCA’s impact on low-income families and the middle class, will make using employer-sponsored health care plans or other forms of health insurance more expensive.
As explained by Reed Abelson and Katie Thomas of The New York Times, this fear is part of what has brought doctors, hospitals and major health insurers together in their simultaneous criticism of the bill. The costs experienced by for-profit health insurers will never return to pre-ACA levels, especially if Medicaid, the nation’s largest health insurer, is dealt the setbacks in funding under the AHCA.
What Does Your Organization Need to Do About the AHCA Today?
Your organization needs to take steps to safeguard against the negative possibilities that could occur if the AHCA becomes law.
If your organization pays for recertification and training among employees, make sure all staff members have completed their proper credentials and training at once. Encourage all employees to recertify their training and credentials now, such as renewing their BLS certifications. This will give your organization some wiggle-room in finding other funding or financial sources to pay for future training programs.
Your organization should also try to limit expansion of programs that receive funding in whole or in part under the ACA, considering all potential impacts across the health care industry, ranging from overhead costs to telehealth programs. This will mitigate any losses incurred if the bill becomes law.
The AHCA current state will change how Americans access health care, and it will have a lasting impact on all generations. More than anything else, your organization needs to still be cautious and vigilant in the coming months, and if the bill does pass, we will create a new article that will provide intense, immediate direction for how your organization can respond and meet the challenges presented by new legislation.






Leave a Reply