Your cart is currently empty!
The Value of the Opioid Algorithm—Saving Lives and Managing Epidemiology
The opioid epidemic is a global problem and burden on health care. According to CNN.com, roots of the problem traces back to the release of a proposed newer, safer alternative to traditional painkillers in the 1990s, OxyContin. Regardless of how it was originally marketed, the use of newer opioids represented a change in how health care providers perceived pain management. Since the 1990s, science has revealed a darker side of the equation. Opioids possess significant addictive qualities, giving rise to their vast abuse.
 As the epidemic grew and damaged lives, not to mention the death toll, it became clear a new approach to treating the problem was necessary. The opioid algorithm is this approach, combining life-saving skills with overdose-specific guidelines to increase survival chances.
As the epidemic grew and damaged lives, not to mention the death toll, it became clear a new approach to treating the problem was necessary. The opioid algorithm is this approach, combining life-saving skills with overdose-specific guidelines to increase survival chances.
Now, the opioid-specific algorithm was created in 2015, reports ILCOR, to provide health care providers with direction on how to approach and treat those suffering from a life-threatening overdose. While the traditional standards for Cardiopulmonary Resuscitation (CPR) and Basic Life Support (BLS), focused on achieving stability, failure to treat opioid overdose itself increased mortality. Think about it. Unless the health care professional recognizes the symptoms and signs of opioid overdose, actual diagnosis may not take place until a positive laboratory test revealed the presence of opioids. Because of opioids’ effects on body systems, including the respiratory and cardiac systems, recognizing an opioid overdose is essential to survival.
Instead of shifting blame and trying to uncover why someone may abuse opioids, health care professionals today need to understand how the opioid algorithm saves lives, how to apply it and a few other practices to ensure optimum treatment outcomes after its use.
Opioid Overdose Statistics
The opioid epidemic gained a negative reputation as a disease that arose from nowhere. Statistics tell a different story. According to the Centers for Disease Control and Prevention, drug overdoses led to the deaths of more than 700,000 people between 1999 and 2017. In addition, more than 70,000 drug overdose deaths occurred in 2017, and the overwhelming majority, 68%, involved an opioid overdose. Risk of overdose has increased six-fold since 1999, and every day, 130 Americans die from opioid overdose.
Different drugs are responsible for the rise in opioid overdoses. In the early 1990s, prescribers began increasing the use of opioid pills as a means of controlling pain. In 2010, the epidemic approached a new height as heroin became the leading killer in the epidemic.
Finally, 2013 brought the most significant increase, following the use of synthetic opioids, such as illicitly manufactured fentanyl. Unfortunately, legislation governing the sale of medications through the Internet make isolating and stopping the epidemic more difficult. While politics continue to debate the legitimacy of the epidemic and how to best manage it, health care professionals have an option.
The application of the opioid algorithm can reduce the risk of mortality by arming caregivers with the knowledge to recognize the signs of opioid overdose, treat it with naloxone and follow through with subsequent resuscitation steps. In traditional care environments, opioid overdose was not included as a reversible cause of arrest. Although, the symptoms of an overdose, such as decreased respiratory capacity or hypotension, are included.
To ensure health care providers do not overlook a cause that cannot be readily identified through the traditional algorithm, the International Liaison Committee on Resuscitation (ILCOR) released the opioid algorithm. It would serve to bridge the divide between symptom recognition and proper treatment.
How to Use the Opioid Algorithm
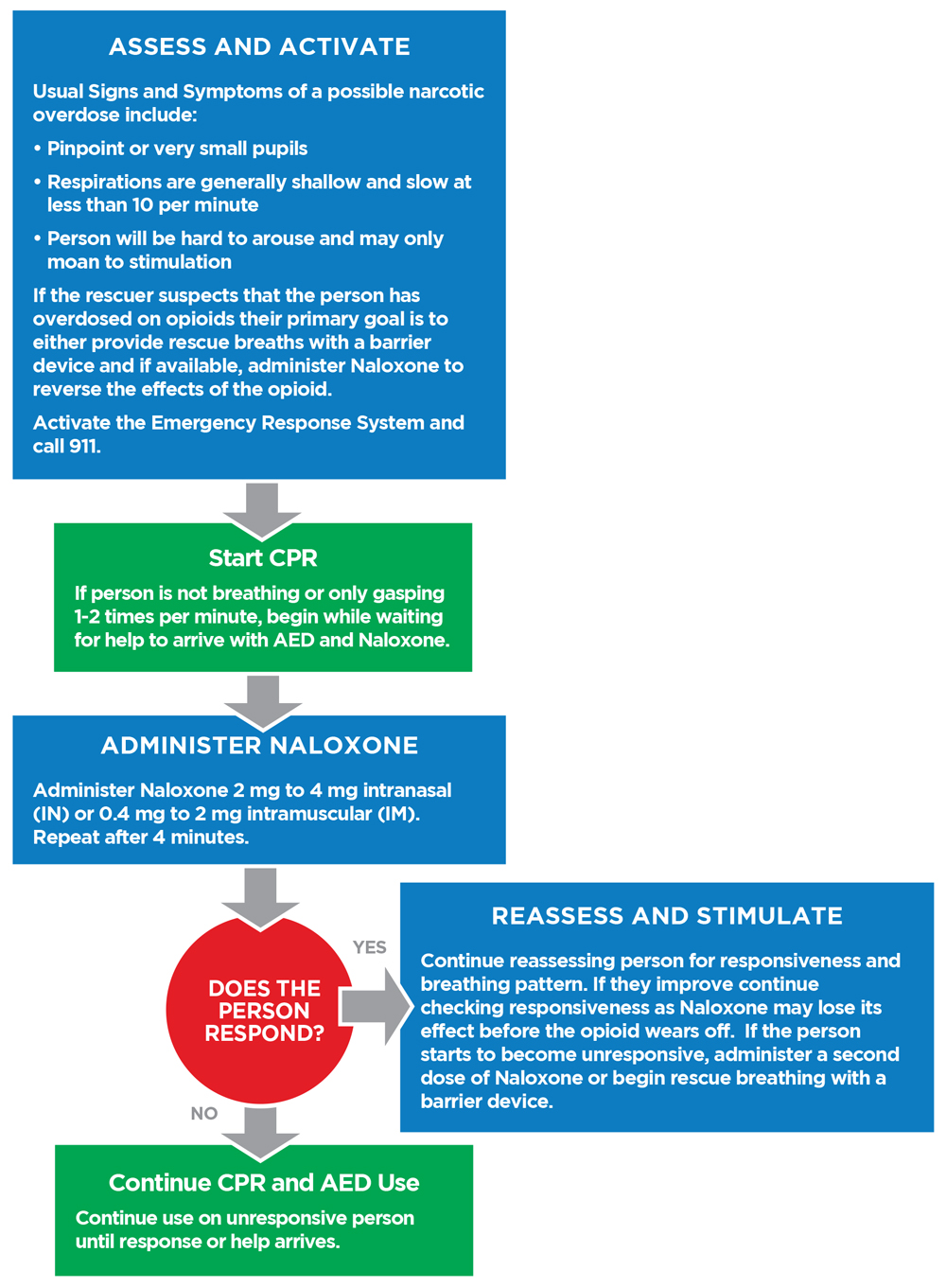
The algorithm follows seven steps that will increase the chances of survival following opioid toxicity or overdose. These include:
Step 1: Assess/ Activate the Chain of Survival
The opioid algorithm requires the rapid identification of symptoms associated with opioid overdose. As explained by MedlinePlus, symptoms may include:
- Altered mental status or lethargic.
- Pinpoint pupils.
- Extreme pallor and clammy skin.
- Inability to control one’s own body or experiencing extreme limpness.
- Excessive vomiting or making noises like gurgling, choking or gasping without a reasonable explanation.
- The appearance of a purple or bluish hue on the fingernails or lips, reflecting decreased cardiac output.
- Inability to be awakened or speak.
- Diminished breathing or slow heart rate.
- Respiratory or cardiac arrest.
When the symptoms appear, it is necessary to activate the chain of survival. Depending on your location, this may involve calling 911, activating your facilities code team or shouting for help. If you are alone, attempt to get another person’s attention to assist with activating the chain of survival, most especially if you are unable to reach 911 on your own device.
Step 2: Start CPR
When recognizing the signs of opioid overdose, it will be necessary to begin the steps of CPR. However, the opioid algorithm advises to begin CPR only if the person is unresponsive, not breathing at all or gasping. When performing CPR alone, continue to perform CPR for a period of two minutes. At this point, it is acceptable to leave the person momentarily to contact 911. In addition, obtain the automated external defibrillator (AED), provided one is available, as well as naloxone.
Step 3: Administer Naloxone
Administering naloxone can feel overwhelming. For those that lack the licensure to routinely administer medications, administering this medication represents a significant change in basic skill set. However, it is essential that the victim receives the medication as soon as possible. Furthermore, naloxone is generally given via a nasal spray or injection into the muscle.
The intranasal delivery is 2 mg in each nostril total of 4mg. The intramuscular injection is 04.mg to 2 mg.
Until help arrives, continue to re-administer naloxone every four minutes if necessary.
Step 4: Assess Responsiveness
After administering naloxone, the opioid algorithm advises to reassess responsiveness of the victim. If the victim begins to breathe regularly, moans or moves purposely, it is appropriate to move forward to step five. However, a lack of responsiveness warrants a return to step two, continuing CPR and BLS until help arrives or the victim becomes responsive.
Step 5: Stimulate and Reassess
Even though the person has exhibited a sign of responsiveness, it is important to maintain control over the situation and close vigilance. Attempt to stimulate the person, asking them to move, respond to questions, talk or perform another simple task. The goal is to keep the person awake and engaged. This would effectively eliminate the need to continuously check for a pulse and assess breathing.
At any point, the person could reenter the state of unresponsiveness. This is the result of the continued release of opioids into the bloodstream following ingestion. Depending on the mode of ingestion, the person could easily reenter the overdose state. Thus, it is important to maintain a close watch and respond accordingly.
If the person returns to an unresponsive state or begins to exhibit the signs of respiratory distress, such as gasping or respiratory arrest, return to step two.
Step 6: Move Into the CPR and BLS Algorithm
The next step is the addition of routine CPR and BLS skills to the algorithm. This may include the use of an AED, following the instructions for pad placement per the device and administering a shock if the person enters cardiac arrest with a shockable rhythm. In addition, follow the standards for two-person CPR, and switching between chest compressions and administering rescue breaths.
For those following the two-minute practice of administering chest compressions and switching places with a second responder between administering rescue breaths, the specification for the administration of naloxone every four minutes can be easily tracked. Simply administer naloxone after completing two switches.
Step 7: Follow Steps for Post-Resuscitation Care
The final step in the opioid algorithm is not necessarily spelled-out within what the ILCOR released. However, it is essential to maximizing chances of recovery. Health care professionals should follow the routine post-resuscitation care guidelines for someone that has suffered either cardiac or respiratory arrest. This includes the ongoing treatment of reversible causes of arrest, and while naloxone provided the immediate mechanism of action to treat the reversible cause of arrest, the process lacks value if not applied to help the person treat their addiction. Essentially, following the post-resuscitation care guidelines for monitoring, management of other conditions and support implies a need to help the person find and obtain follow-up care with an appropriate organization or treatment facility.
Additional Concerns Following Use of the Algorithm
 Even while a patient remains in a health care facility after an opioid overdose, great risk remains. Health care professionals need to understand a few additional concerns following the use of the algorithm to ensure the safety of the victim as well as their own.
Even while a patient remains in a health care facility after an opioid overdose, great risk remains. Health care professionals need to understand a few additional concerns following the use of the algorithm to ensure the safety of the victim as well as their own.
Return of Reversible Causes of Arrest
Prolonged use of opioids can have an adverse effect on the function of normally healthy body tissues. The cardiovascular, respiratory, and nervous system may have grown accustomed to the presence of opioids, reflecting the onset of addiction. In other words, those that have suffered an opioid overdose may exhibit an increased risk of hypertension, trauma or other incidents that would contribute to the return of cardiac or respiratory arrest.
Subsequent Use of Opioids While in the Facility
Those suffering from an addiction may fail to recognize the adverse impact of opioids on their lives. The powerful nature of substance abuse means those that have endured and survived an overdose may have an increased likelihood of using the same substances while still in your facility. Thus, the risk of a subsequent opioid overdose will remain despite having received naloxone as part of the response.
Inability to Ensure a Patient’s Safety
Depending on the severity of addiction, another concern exists in the form of a patient’s inability to guarantee their own safety. Withdrawal symptoms may occur, including aggression and self-injurious or suicidal behaviors. At this point, it falls to the health care professionals to ensure a patient’s safety.
Moreover, those that suffer an opioid overdose may use any means necessary to obtain subsequent opioids, as noted in the first concern. This may include asking family members, friends or other individuals to bring opioids, which may be in either pill or liquid form, to the facility. It may be necessary to revisit the standard medical supplies and medication brands to separate non-facility items, such as syringes, that a victim may possess.
In fact, a contributing health care professional in Texas experienced these concerns first-hand when a patient had discarded a used syringe in the bathroom waste bin that did not possess the same markings or coloration of the facility. Upon presentation to the charge nurse, a decision was made to guarantee the patient’s safety and ensure adherence to medical advice. This included placing a staff member in the room to maintain a vigil over the patient. This provided a two-fold effect, resolving the hospital of liability for the presence of opioids in the patient that could have been used in future legal matters. Moreover, it insured the patient’s safety by preventing the subsequent use of opioids, which effectively lowered the risk of a subsequent overdose.
Following the event, the professional used poster-board and excess supplies to create a chart, one-stop view of facility-approved and -used syringes and basic pill images. This served to ensure that untrained or new staff could recognize when a syringe or other pill just simply did not align with the facility-specific medications and supplies.
Know the Value of the Opioid Overdose Algorithm to Save Lives
The ILCOR algorithm for managing opioid overdose leverages a sequential chain of survival that is comparable to the basic CPR steps. However, it focuses on treating opioid overdose, as well as recognizing it as a reversible cause of arrest, and proceeding through the remaining steps of resuscitation. Since the opioid epidemic continues, health care professionals need to understand the opioid algorithm and the symptoms associated with opioid overdose. Chances are good they will encounter it, especially in areas responsible for urgent care, emergency care, and other settings, not to mention the recent increase of overdoses in everyday settings.
Have you ever been involved in responding to someone suffering from an opioid overdose? If so, share your experiences and this article to social media now. Remember the chance of survival following an overdose is only as strong as the skills and knowledge of those that apply the algorithm in conjunction with the CPR and BLS standards. So, enroll in your life-saving skills course now.










Leave a Reply