Whether dealing with a fast heartbeat or a more complex arrhythmia, these vagal maneuvers offer a quick, non-invasive way to manage your patient’s condition. In the medical tech-dependent emergency medicine environment, it’s easy to forget about some of the practical solutions you have at your disposal. The simplest solution is often the best, and knowing when and how to use vagal maneuvers can make all the difference.
These straightforward techniques can stabilize your patient, buying your patient valuable time for further treatment.
What Are Vagal Maneuvers?
Vagal maneuvers are simple, non-invasive techniques that you can use to manage specific types of arrhythmias in your patients. These work by stimulating the vagus nerve, which controls your patient’s heart rate.
This makes vagal maneuvers particularly effective in treating certain arrhythmias like supraventricular tachycardia (SVT), a rapid heart rhythm above the ventricles. Plus, because you can perform each technique quickly on your patient without needing medication, you get a highly effective, non-pharmacological approach to emergency care.
Every Emergency Medicine Professional Must Master These Techniques
When your patient presents with a sudden arrhythmia, which could be supraventricular tachycardia (SVT), these maneuvers are an early step in both diagnosing and managing that irregular heartbeat. If it doesn’t work, you can always move to more aggressive treatments like medications or electrical cardioversion. But if you could help your patient avoid all that and any potential side effects, wouldn’t you?
Slowing the heart rate through vagal nerve stimulation can help stabilize your patient’s condition. This creates a window of opportunity for further evaluation and treatment when seconds matter.
Vagal maneuvers are especially valuable because you can perform them quickly and without specialized equipment. This makes them ideal for use in hospital settings and the field. For paramedics and other first responders, the ability to perform these maneuvers on the spot can be a critical factor in patient survival. Before you can say, “hook up the ECG”—which you still need to do by the way—you could have already restored a normal heart rhythm.
Even in a hospital environment, where more advanced interventions are readily available, vagal maneuvers are often the preferred first-line treatment due to their safety and efficacy.
What’s more, incorporating vagal maneuvers into your team’s ACLS protocols aligns with the overall goal of minimizing your patient’s risk while maximizing the chances of a positive outcome. Why not test your skills with this online Megacode for SVT to see how you or your team would respond?
These maneuvers are not just about treating symptoms. They target the underlying cause of the arrhythmia. And they offer a more holistic approach to patient care.
At Save a Life, our ACLS courses emphasize the importance of these maneuvers, ensuring that you’re well-equipped to use them effectively in your practice. It doesn’t matter if you’re a patient-centered nurse keeping abreast of the latest evidence-based care or a paramedic learning how best to adapt to the uncertainties of your day. When you complete your ACLS certification online, you gain valuable knowledge to save lives and improve patient outcomes.
How Effective is Vagal Maneuver in ACLS?
I don’t want to give the impression that vagal maneuvers work on every one of your patients every time. That is not what makes these so helpful in your practice. They’re important because you can perform them quickly. They will sometimes work, particularly with SVT. Then, you can progress to more invasive interventions when they don’t work.
A randomized controlled trial titled “Initial and Sustained Response Effects of 3 Vagal Maneuvers in Supraventricular Tachycardia: A Randomized, Clinical Trial” divided 98 admitted SVT patients into groups based on type of maneuver (Nih.gov):
- Standard Valsalva maneuver (sVM)
- Modified Valsalva (mVM) maneuver
- Carotid sinus massage (CSM)
I’ll discuss how to perform each of these maneuvers in a subsequent section, but first, I will discuss the findings.
During the study, they saw success rates of:
- 44% for Modified Valsalva (mVM) maneuver
- 24% for Standard Valsalva maneuver (sVM)
- 9.1% for Carotid sinus massage (CSM)
A meta-analysis of randomized controlled trials that had over 2000 participants supports the previous study’s findings. Modified Valsalva is the most effective technique when compared to carotid sinus massage. That doesn’t mean you shouldn’t have all of these maneuvers in your toolkit. However, it does suggest that when you can perform mVM, that’s the evidence-based option (NIH.gov).
The Physiology of Vagal Maneuvers for SVT
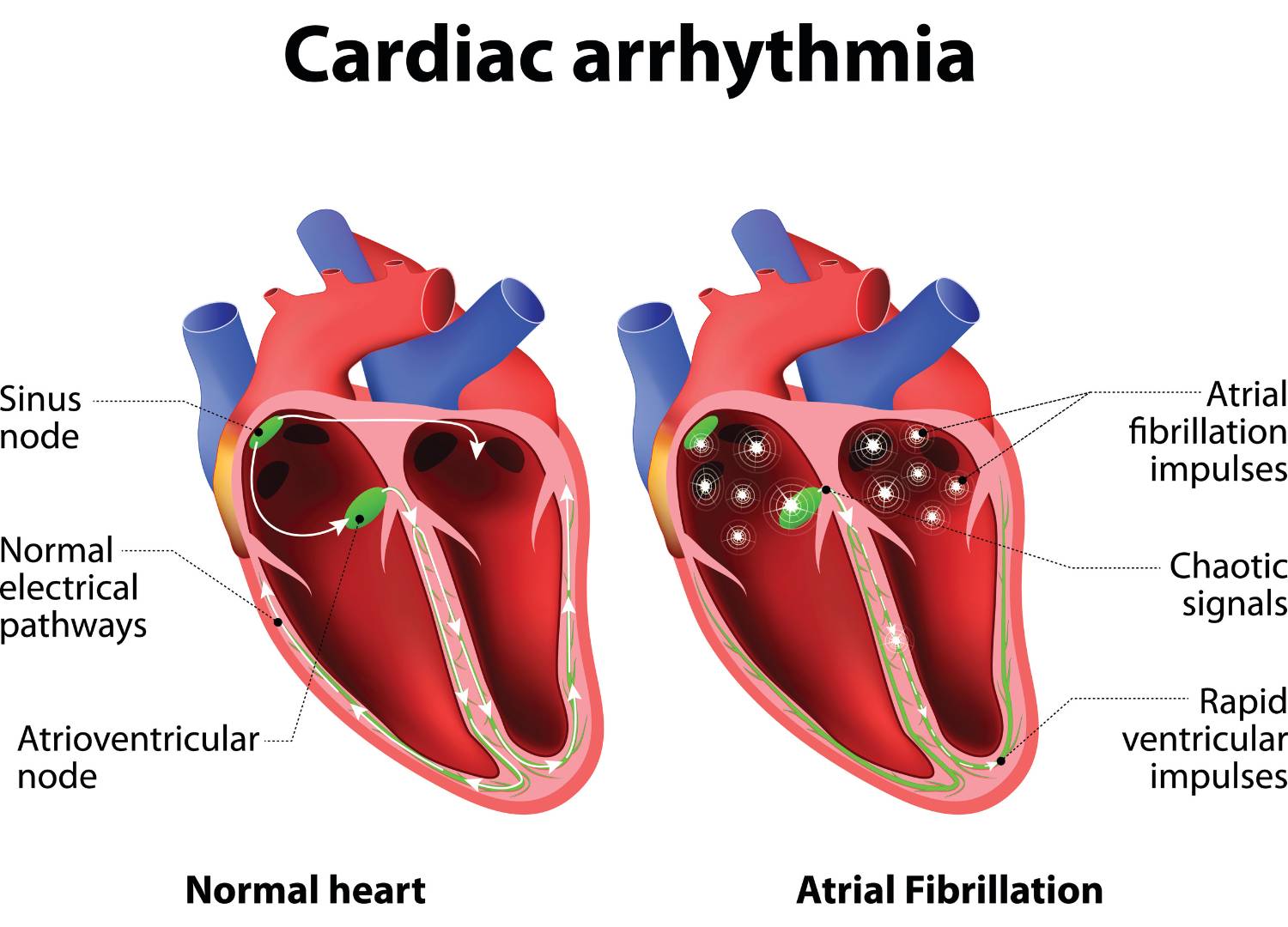
The vagus nerve is part of the parasympathetic nervous system. It’s crucial in controlling your patient’s heart rate. By activating this nerve, vagal maneuvers can slow down your patient’s heart conduction system, particularly the atrioventricular (AV) node, the heart’s pacemaker.
When the vagus nerve is activated, it reduces the sympathetic nervous system’s activity, which includes fight-or-flight responses like an elevated heart rate. At the same time, it increases parasympathetic activity, which tells the heart to slow down.
This results in a decreased heart rate, which can terminate the arrhythmia. For example, in the case of SVT, the AV node is often the re-entry point for the arrhythmia. Slowing or blocking it with a vagal maneuver can terminate your patient’s arrhythmia in this instance.
Vagal Maneuvers in the Diagnosis and Treatment of Arrhythmias
As I mentioned, vagal maneuvers are not just therapeutic. They are also diagnostic. When you use these techniques on your patient, the response can provide valuable information you can use to decide what to do next.
For instance, if the heart rate slows or the irregular heartbeat stops after a vagal maneuver, it’s more likely that the arrhythmia is SVT rather than VT. This is crucial in guiding your treatment approach.
Just take a look!
- If a vagal maneuver slows or stops the SVT, treatment may include adenosine, which further slows AV node conduction. If your patient’s rhythm does not respond to the maneuvers, additional medications like beta-blockers or calcium channel blockers may be used. Then, you would consider cardioversion if your patient becomes unstable.
- If the heart does not respond, it will likely be VT. Ventricular tachycardia is more serious and often requires immediate intervention. If the patient is stable, you will administer antiarrhythmic drugs like amiodarone if it’s within your scope of practice. If unstable, synchronized cardioversion becomes your primary treatment. Note: VT can quickly progress to ventricular fibrillation, a life-threatening condition.
Aren’t you glad you used this diagnostic technique to find out fast? As much as I appreciate medical technology, and I know you do, too, this practical technique got the job done faster and better.
In addition to treating SVT, vagal maneuvers can be useful in other scenarios, such as helping to diagnose the presence of an accessory pathway in Wolff-Parkinson-White syndrome, which is a congenital heart condition that causes abnormal conduction between the atria and ventricles (Nih.gov).
When to Use Vagal Maneuvers in ACLS
This technique is appropriate after you’ve ruled a few things out:
- Wide QRS > or = to .12 seconds on the 12-lead ECG
- Hypotension (low blood pressure)
- Acute altered mental status
- Signs of shock (dilated pupils, sweaty/cold skin, gray or blueish lips or nails, etc)
- Chest pain
- Acute heart failure
If none of these are true, vagal maneuvers are your next course of action.
Please review the evidence-based ACLS algorithm for tachycardia for more details, as I’m giving a high-level overview.
What Are Examples of Vagal Maneuvers?
Here are some common vagal maneuvers you can use in your practice:
- Standard Valsalva Maneuver: Have your patient take a deep breath and bear down as though trying to have a bowel movement. This increases intrathoracic (chest) pressure and stimulates the vagus nerve.
- Ice Water Facial Immersion: Applying ice-cold water to your patient’s face can also trigger the vagus nerve. This is sometimes referred to as the “diving reflex.”
- Gag Reflex Stimulation: By inducing a gag reflex, you can also stimulate the vagus nerve. However, this one may not be the most pleasant of your options.
- Modified Valsalva Maneuver (mVM): Similar to the standard Valsalva, but with an added component. After the initial strain, lay the patient flat and elevate their legs. This modification can increase the effectiveness of the maneuver by enhancing venous return, leading to a greater drop in heart rate, as noted in the aforementioned study.
- Carotid Sinus Massage: Gently massage the carotid artery on one side of your patient’s neck. This stimulates the baroreceptors, which activate the vagus nerve, helping to slow the heart rate.
It’s important to perform this maneuver carefully, especially in older patients, to avoid complications. A study of 1000 patients over 50 with unexplained falls and syncope (fainting) found that 9 of the 1000 (roughly 1%) experienced neurological disturbance following a five-second session. Symptoms included pins and needles. numbness, lower limb weakness, vision problems, and “feeling drunk”. This didn’t sound severe to me until you learned that these symptoms lasted up to 24 hours with no further complications (Nih.gov).
However unlikely this is, it’s useful information for any attending nurse, doctor, or first responder to be aware of when you’re treating an older patient.
How to Do Vagal Maneuvers: Step-by-Step Guide
I’ve created this step-by-step guide to help you through the process for each technique:
Standard Valsalva Maneuver (sVM):
- Step 1: Have your patient sit or lie down comfortably.
- Step 2: Instruct them to take a deep breath.
- Step 3: Ask your patient to bear down as if trying to have a bowel movement and instruct them to hold that position for 15 seconds.
- Step 4: Monitor your patient’s heart rate during and after the maneuver. You should see a drop in heart rate if the maneuver is successful.
Modified Valsalva Maneuver (mVM):
- Step 1: Start with the steps of the Standard Valsalva Maneuver.
- Step 2: After the patient bears down, lay them flat and raise their legs to 45 degrees for 15 seconds.
- Step 3: Return the patient to a seated position.
- Step 4: Observe for any changes in heart rhythm.
Carotid Sinus Massage (CSM)
- Step 1: Have your patient lie down with their head slightly turned away from the side you will be massaging.
- Step 2: Gently apply pressure to the carotid artery located in the neck, just below the jawline.
- Step 3: Massage for about 5-10 seconds while monitoring your patient’s heart rate.
- Step 4: Repeat on the other side if necessary. But never massage both sides simultaneously.
Ice Water Facial Immersion
- Step 1: Prepare a basin of ice-cold water.
- Step 2: Instruct your patient to hold their breath.
- Step 3: Submerge your patient’s face in the cold water for a few seconds.
- Step 4: Monitor the heart rate after the maneuver.
Getting Your ACLS Certification
Vagal maneuvers are just one type of helpful technique you learn about in Advanced Cardiac Life Support (ACLS) training. You’ll gain access to the latest in evidence-based ILCOR-approved ACLS guidance with videos, algorithms, study guides, a useful app, plus Megacodes to test your knowledge in specific situations. Then, take the practice test to see if you’re ready to get ACLS certified. You can earn medical education credits 100% online and gain valuable, life-saving skills.
Frequently Asked Questions About Vagal Maneuvers
What Does the Vagal Maneuver Do?
You can use them to stop episodes of stable supraventricular tachycardia (SVT) or to help differentiate SVT from ventricular tachycardias (VT).
These maneuvers cause a vagal response, slowing the electrical impulses traveling through the heart. This slowing effect helps break the cycle of the rapid heartbeat associated with SVT and, in some cases, can return the heart to a normal rhythm without needing medication.
Can Vagal Maneuvers Convert Atrial Fibrillation?
Typically, you perform vagal maneuvers for SVT. In the case of AFib, these maneuvers are unlikely to convert the arrhythmia back to a normal sinus rhythm. However, they may provide some benefit by slowing the heart rate, which can make the arrhythmia less symptomatic for your patient.
Can I Lower My Blood Pressure with a Vagal Maneuver?
While this guide is intended for medical professionals like yourself, anyone can use vagal maneuvers to temporarily lower blood pressure, heart rate, and stress feelings by activating the parasympathetic nervous system. You’re in a high-stress job, so having a self-therapeutic technique like this to ease the stress response (when not in an emergency) is very useful.
Is Valsalva the Same as Vagal Maneuver?
The Valsalva maneuver is a type of vagal maneuver but not the only one. In other words, all Valsalva maneuvers are vagal maneuvers, but not all vagal maneuvers are Valsalva maneuvers.
The Valsalva maneuver specifically involves your patient taking a deep breath, holding it, and then bearing down as if trying to have a bowel movement. This action increases pressure within the chest cavity, which stimulates the vagus nerve and can slow the heart rate.






Leave a Reply