Survival following a cardiac arrest or a major medical emergency, such as stroke, heart attack or trauma, depends on the ability of health care professionals to respond to emergent situations. Although this includes initial treatment in an emergency department, admission to a health care facility in the healing process, especially an intensive care unit (ICU), still carries a risk of mortality. Subsequent cardiac arrest or health problems could develop without warning, contributing to more than 325,000 deaths in the U.S. per year, explains WebMD.com. This is where ACLS Megacodes, which are intense, timed ACLS scenarios that have value in refreshing your ACLS skillset and improving treatment outcomes, make a proverbial splash.
Since ACLS skills’ training may only recur with your licensure renewals, it is important to stay on top of ACLS updates and changes in standards as they occur. The last major update to the ACLS algorithm, published by the International Liaison Committee on Resuscitation (ILCOR), took place in 2015. Even if you were exposed to the changes with your last renewal, it is easy to forget relatively minor changes that can impact cardiac arrest survival. So, Megacodes completion and a thorough review of the changes in the algorithm are key to keeping your skills up to date.
What Exactly Are ACLS Megacodes 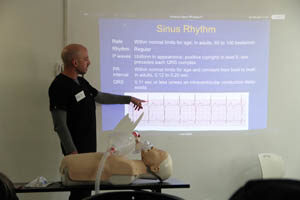
ACLS Megacodes are a series of real-time, hypothetical scenarios that include some, but not all, background information for a hypothetical patient and ask participants to choose the correct, next step in the ACLS algorithm. In other words, Megacodes’ participants are given the opportunity to respond in real-time to a presumed patient. Failure to answer the question correctly will bring up a new box that explains why the chosen answer is incorrect and what it could mean.
Depending on the scenario, participants may also be presented with an EKG strip and asked to interpret and act upon the reading. Depending on the already-completed steps and best practices, one or more answer choices may be appropriate. However, only one answer aligns with the 2015 ACLS updated guidelines. This is similar to the way questions were presented on the NCLEX for nursing licensure.
Although the setup may appear “tricky,” the scenarios are created to mimic the real-world scenarios and critical-thinking required when acting in an emergency. Of course, the Megacodes are not limited to the ACLS survey, so participants must know what medications are appropriate, the time duration in which they can be administered, appropriate dosages, the need to defibrillate, and whether to resume chest compressions. Understanding the right sequence, such as starting chest compressions, administering medications and defibrillation, increases survival, reports Heart.org, and missteps could result in poor cardiac perfusion, extended stress on the cardiovascular system, and increased risk of mortality.
The ultimate goal is to help health care professionals improve their ACLS skills. Of course, understanding the ACLS algorithm and its changes is essential to improving chances of survival.
A Brief Review of the ACLS Algorithm
An effective approach to an acute ailment must begin with the ACLS Survey, reflected in the letters ABCD, including:
- Airway – Maintaining an airway in the unconscious person.
- Breathing – Giving 100-percent oxygen and avoiding over-ventilation.
- Circulation – Evaluation of the rhythm and pulse, starting an IV/IO access and administration of medications as necessary.
- Differential diagnosis – Treating the most likely cause of arrest and subsequent, less likely causes, pausing only to confirm or treat reversible causes.
The algorithm transforms the ACLS survey into a flow of treatments and interventions to reduce mortality risk. It begins with starting CPR and identifying whether a rhythm is shockable or non-shockable, such as asystole or PEA.
If a shockable rhythm exists, administer the shock, and continue CPR for two minutes, during which an IV/IO access is obtained. If the rhythm is not yet shockable, health care professionals must move to administer epinephrine every three-to-five minutes and consider an advanced airway. If the rhythm becomes shockable, then administration of amiodarone, following another two-minute period of CPR, amiodarone may be administered, treating the reversible causes of arrest at the same time.
In the case when the rhythm is non-shockable, the only pathway lies in administering CPR and epinephrine at the given intervals and treating the reversible causes of arrest, including hypovolemia, hypoxia, hydrogen ion build-up, also known as acidosis, hyper- and hypo-kalemia, hypothermia, pneumothorax tension, cardiac tamponade, toxicity, and coronary or pulmonary thrombosis.
Key Changes in the 2015 ACLS Update
The dominant changes to the ACLS algorithm in 2015 are not necessarily major changes to how health care professionals approach individuals in distress. However, several notable exceptions exist, including:
- Complete abandonment of monophasic defibrillators when biphasic defibrillators are available.
- Following manufacturer recommendations for energy level when administering shocks. If not available, maximum doses may be used.
- Specific adherence to the standard one mg dose of epinephrine every three-to-five minutes.
- Immediate initiation of chest compressions.
- Administration of epinephrine as soon as possible for those with non-shockable rhythms, excluding PEA when previous doses of epinephrine have not resulted in a return to circulation.
The administration of epinephrine as soon as possible stands apart from the other changes in the ACLS algorithm. Previous thinking involved the administration of epinephrine viewed epinephrine administration at any point as increasing life expectancy. However, an observational study found non-shockable rhythm survival increased dramatically, especially with neurologically intact survival, when epinephrine was administered within three minutes.
Special Considerations for the Value of Megacodes From an Expert
NHCPS recently had the opportunity to sit down with a Registered Nurse with more than 10 years of experience as a Charge Nurse in a Medical Intensive Care Unit (ICU), now serving as the Education Coordinator for both the Pediatric and Medical ICU at the same, 625-bed hospital. Her first-hand account of the common mistakes health care professionals make in the course of performing ACLS emphasized that studies may not always reveal the true nature of an ACLS response.
Some of the key questions and responses include:
What’s the biggest mistake nurses and nursing ancillary staff make when responding to a Code Blue?
“The biggest mistake, by far, is the tendency to assume every Code Blue is a case of V-Fib. Although it’s a dominant cause of arrest, it is not the only arrhythmia we have to address. There have been multiple incidents where staff did not administer amiodarone properly when running a Code during a shockable rhythm or PEA. It simply does not work.”
Do staff members routinely experience the “fight or flight” response when a Code has been activated?
“All the time. We are trained to respond professionally and promptly, but the body’s natural “fight or flight” response has a way of getting in the way during a Code. Everyone starts to try to take the initiative, and without recurring training, someone will start actions that are not assigned to them. It’s the classic “too many chiefs” scenario, so knowing exactly how to work as a cohesive unit is key.”
How often do staff members participate in Mock Codes, and how do real-life Mock Codes affect employee performance and treatment outcomes?
“In the ICU, we tried to run a Mock Code at least once every six months. It was impractical. The acuity of our patients required all our attention. Spending time away from critical care patients to perform a drill on a mannequin can be a disaster. In multiple cases, not all staff members were able to participate. The most common cause of non-participation was patients that were on a cardiac balloon or other treatment that required constant eye-contact. Stepping away is not possible. The only other option was to go to a skills’ fair on our days off or after clocking out.”
Speaking of Mock Codes, did your staff ever participate in digital, computer-based Mock Codes? Also, have you had an opportunity to review the ACLS Megacodes scenarios? If so, what is your opinion on their value to the critical-care professional?
“We had a few digital options, but they were mostly simple tests. The test involved the most basic of questions, like “what’s the proper dose of epinephrine for an adult, or which of the following is a non-shockable rhythm?” In multiple cases, we even had the answer choices already passed around the unit. They weren’t timed, and if you got an answer wrong, you simply had to click on the correct answer to change it.
Megacodes are completely different. They actually give us a scenario, putting our imaginations to work. We had to think about the answers, not just pick one. We had to look at the EKG strip, recognize the rhythm, decide what to do, and read the question. The time ran out faster than I realized with the first one. I knew the answer, but I zoomed into the strip to see. Next thing I knew, the timer ended, and I couldn’t finish it. I can admit that I took it at least three times before I was able to answer each question right and within the time limit. It makes you think in the same way a real code does.”
Did you find the information in the multiple Megacodes helpful, and what do you think Megacodes could mean for improving competency on the floor?
“Megacodes are a great resource for new and experienced nurses. I thought they were focused exclusively on cardiac arrest, but they also touched on different arrhythmias, stroke, and a STEMI [sustained elevation myocardial infarction]. In the Medical ICU, we didn’t see many STEMI patients. They were usually sent to Cardiac ICU. It was an easy way to review the steps necessary in treating these life-threatening scenarios.
I believe that using Megacodes throughout training for staff members in critical care could lead to endless possibilities in how we approach patients and continuing education. During lulls in the shift, which are rare, the scenarios’ three-minute limit means staff members could complete the scenario in less time than it takes to go to the restroom. It wasn’t a distraction while at work. Even during busy days, the ease of accessing Megacodes without logging in to a company network could mean reviewing ACLS on a day off.”
You mention the short nature of Megacodes? Do you think they thoroughly covered the ACLS algorithm and changes with the last ILCOR update?
“Yes. They were broken into the major issues leading to cardiac arrest. For the STEMI scenario, I liked that it went outside of the ACLS steps, including the mention of administering aspirin and proceeding with the ACLS Survey for someone with a heart attack, opposed to another case of cardiac arrest. Another scenario touched on something that was updated in 2015 that I still have a hard time remembering, the change in administering amiodarone. Now, I can’t get that screen out of my head. It keeps playing over and over, like a movie. I think the scenarios will help new and experienced nurses commit new information about ACLS to memory, even better than in-person practice too.”
How Will the Future of Megacodes Evolve
 The future of ACLS Megacodes is filled with opportunities for improvement in critical care. With less than two years until the next ILCOR update, which will take place in 2020, committing the 2015 updates to memory and putting knowledge to the test through these scenarios will be essential to the survival of those in cardiac arrest.
The future of ACLS Megacodes is filled with opportunities for improvement in critical care. With less than two years until the next ILCOR update, which will take place in 2020, committing the 2015 updates to memory and putting knowledge to the test through these scenarios will be essential to the survival of those in cardiac arrest.
Since critical care is stressful and time-intensive, health care professionals can leverage the power of Megacodes to review their skills and become more proficient, much like the Charge Nurse in the interview. Although speaking on the condition of anonymity, she did leave us with a lasting thought:
This is definitely going in my list of courses to have the staff complete.”
Her desire to share Megacodes with her team members highlights their value, so follow her example by sharing this post and your thoughts on Megacodes to social media. Furthermore, remember to put your skills to the test to get the refresher you need with the ACLS simulations now.






Leave a Reply