Knowing to respond to someone in distress or cardiac arrest is essential for health care professionals. A misstep could result in permanent injury or death, and cases involving children in distress place a heavier burden on caregivers. Pediatric Advanced Life Support (PALS) is the go-to solution for treating children in distress, and PALS Megacodes, which are realistic, scenario-based PALS training quizzes, are an effective way to reduce the uncertainty associated with providing care to children in respiratory or cardiac stress.
 As explained by ILCOR, more than 5,000 children experience a non-traumatic cardiac arrest in the U.S. each year, but children may experience respiratory distress or cardiac arrest as the result of a trauma as well. In fact, cardiac arrest is a frequent result of respiratory failure in children, explains Medscape. Prolonged respiratory distress can result in additional cardiac stress and contribute to lower cardiac output, which can have lasting effects if not treated properly. Unlike adults, children in need of PALS care are less likely to suffer from chronic medical illnesses that result in cardiac or respiratory distress.
As explained by ILCOR, more than 5,000 children experience a non-traumatic cardiac arrest in the U.S. each year, but children may experience respiratory distress or cardiac arrest as the result of a trauma as well. In fact, cardiac arrest is a frequent result of respiratory failure in children, explains Medscape. Prolonged respiratory distress can result in additional cardiac stress and contribute to lower cardiac output, which can have lasting effects if not treated properly. Unlike adults, children in need of PALS care are less likely to suffer from chronic medical illnesses that result in cardiac or respiratory distress.
That fact does not negate the need to know how to respond to a variety of causes of distress. Thus, health care professionals need to consider completing Megacodes to identify their strengths and weaknesses in PALS and provide the best care possible.
An Overview of PALS Megacodes
Unlike Advanced Cardiac Life Support (ACLS) Megacodes, PALS scenarios are a series of timed quizzes presenting a hypothetical child in distress. The simulation is conducted online, and anyone can access it without registering or completing lengthy paperwork.
Users simply access Megacodes, and the countdown timer begins. Most of the scenarios have an allotted time of three minutes, which mirrors the amount of time spent in conducting the ABCs of PALS and treating the child in need.
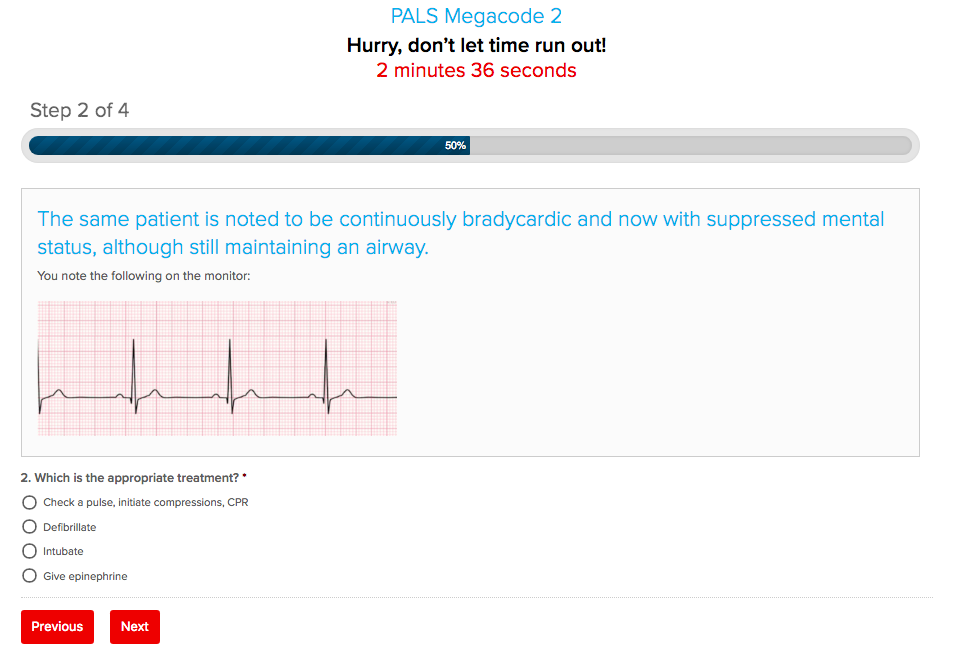
Depending on the simulation, the questions may build upon one another to show the progression of distress in children. In other cases, the simulation may present a new, hypothetical child experiencing different symptoms. An electrocardiogram (EKG) strip may be presented, but the question may not reflect an interpretation of the reading.
The onus of recognizing the rhythm or arrhythmia and pairing it with the listed symptoms is on the user. Answer choices may offer similar solutions, but only one answer is truly correct. As part of PALS training, this set of Megacodes will have answers that are correct for performing ACLS on adults.
Some of the situations denoted within the PALS simulations include:
- Bradycardia, which is a decreased heart rate.
- Tachycardia, which is an increased heart rate.
- Poor cardiac output, which may be the result of both bradycardia
- or tachycardia, as well as other causes.
- Diminished respiratory capacity or severe respiratory distress
- Medical distress resulting from a recent illness, like diarrhea
- and dehydration.
- Trauma, including accidents and injuries, which may precipitate sudden cardiac arrest in children, reports the Pediatrics.AAPublications.org.
This series of quizzes also keeps users on the edge of their seats by switching the age group of children throughout the simulations. This reflects the wide variety of ages that a caregiver may be presented with when providing life-saving support to children.
Benefits of Completing Pediatric-Focused Megacodes
Children lack the metabolic capacity to survive major health events, like respiratory or cardiac distress, without immediate intervention. Although time is of the essence in all cases of respiratory and cardiac distress, regardless of age, providing the right care at an even faster pace to children will mean the difference between life and death.
Completing the PALS scenarios helps health care professionals improve their skills with the following:
-
- In-depth review of the PALS algorithm. Unlike the ACLS algorithm, the PALS algorithm focuses on the uniqueness of administering advanced life support to children. The algorithm is specific to post-resuscitation care, cardiac arrest, tachycardia, bradycardia, and pediatric basic life support (BLS). Since the causes of childhood cardiac arrest are often the result of trauma, understanding the key treatment differences in reversible causes of cardiac arrest is essential to providing quality care. This includes treating for shock, trauma, and arrhythmias. Children in distress may still require CPR and life-saving measures even a faint pulse can be found. Health care professionals must be able to recognize a definite pulse within 10 seconds. If no pulse can be identified, caregivers should begin CPR. This takes a higher priority over identifying the causes of distress.
- Ability to manage response alone or with others present. Knowing how to respond when alone is a key step in the chain of survival. Although those in the health care facility will have access to other trained professionals for help, experiences outside of the care setting may involve performing PALS without the aid of others. In children, time lost trying to get assistance can mean the difference between life and death to a higher degree. The PALS simulations take this into account, questioning users on the appropriate course of action when administering support alone and with others present. Also, the ratio of compressions to rescue breaths differs among child age groups. Failure to adhere to the standards diminish survival chances.
- Identification of the causes of lethargy, poor cardiac output, loss of consciousness, and cardiac arrest in children. Childhood trauma and poor cardiac output may be the result of a temporary or ongoing illness and its symptoms. For instance, a child with decreased consumption of fluids and diarrhea will be more likely to enter tachycardia, and although the initial assumption would be to treat the tachycardia, the best course of action is to correct the imbalance contributing to the increased rhythm. On the opposite side of the spectrum, a child experiencing severe bradycardia may quickly slip into a CPR-requiring pulse. Any pulse below 60 warrants CPR, and this is denoted multiple times in the scenarios. Therefore, caregivers can learn when to administer CPR and life-saving measures when a pulse can be felt.
- Experience in reading and interpreting EKG strips. In non-care settings, accessing an EKG or AED may not be possible. In instances where an EKG can be performed, the ability to correctly interpret EKG results is essential to following the PALS algorithm. Also, EKG results and best treatment actions differ from those of adults. For instance, attempting cardioversion from tachycardia takes precedent over administering a shock. It may not seem like a major change in response, but it makes all the difference to the chances of survival for the child.
- Review of medication administration for cardioversion and in conjunction with CPR. Medication administration in pediatric doses is another great benefit of completing the PALS Megacodes training. Medication dosages are often based on weight and age. In adults, the medications are relatively standard, but child doses depend on the age and weight of the child. Incorrectly administering adult doses could have disastrous effects for the child, not to mention obstruct the effectiveness of PALS. Similarly, the training scenarios help caregivers learn the maximum dosages for medications used to treat causes of distress, including epinephrine, atropine, adenosine, and amiodarone, among others. It is important that caregivers continue CPR and moving through the PALS algorithms even while administering medications due to the duration spent drawing up medications.
- Review of shock levels and frequency in caring for children. Administering electrical shocks for shockable rhythms is a complicated process in children too. The scenarios presented within Megacodes focus on recognizing when a shock is beneficial and its level. For example, administering 0.5 to 1 J/Kg. Again, the nature of childcare goes back to knowing the weight of the child in distress.
- Assessment of the best way to establish effective airways. Establishing an advanced airway in unresponsive children may be easier, but in conscious children that require additional oxygen, it may not be possible to establish such airways without increasing the risk of cardiac arrest. Children have a higher propensity to gag and vomit when an endotracheal tube is placed while conscious, which may lead to panic, severe cardiac stress, and aspiration, further increasing mortality. This is another fact that may go unnoticed in learning more about PALS without completion of Megacodes.
Megacodes and Their Role in Teaching Nursing Students About the Hardest Parts of Health Care
Any discussion on the role of providing life-saving support to those in need will elicit an emotional response. Times will exist when even the best care is insufficient to ensure survival, but the emotional and physical toll resulting from this circumstance involving children will be greater. Administering PALS care correctly keeps families together and builds strong relationships with your peers.
Learning the proper steps in PALS through scenario-based training acts as a buffer to learning how to respond to the most vulnerable people in society, children suffering from distress and their parents, family members, friends, and direct caregivers.
It is a difficult subject to approach for new and inexperienced health care professionals and nursing students. Separating the need to provide emotional support to those affected by the immediate need to intervene as a health care professional will be among the most challenging events of a career. However, prospective and current students must learn to recognize that their actions will have a direct bearing on the survival of the child and the emotional well-being of the child’s family members.
Completing Megacodes helps to build another vital skill in administering life-saving care—a strong ability to communicate clearly and thoroughly. Parents and family members of children in distress will be the link between understanding the child’s recent behaviors or activities that may have precipitated the current situation. This may include recent illnesses, injuries, or other activities, like playing in a cotton field.
Every detail is of vital importance. Children can get into precarious situations even while under direct supervision. An insect bite or exposure to certain foods can trigger anaphylactic shock, leading to cardiac and respiratory distress. A minor scrape or bruise may only reflect the surface wound or injury, and since children, especially very young children, maybe incapable of expressing themselves, the ability to carefully listen to parents will mean the difference between life and death.
The PALS response steps include treatment of the reversible causes of distress, which are identical to the reversible causes of distress in the ACLS algorithm. These include:
- Hypovolemia, which implies an inadequate level of fluid in the body, resulting in decreased cardiac output and perfusion.
- High levels of hydrogen ions, also known as acidosis, resulting from respiratory distress or metabolic conditions.
- Hypothermia, resulting from exposure to the elements, not just the cold. Hypothermia may occur in relatively warm temperatures of around 60 F with prolonged exposure or when wet.
- Hypo- and hyper-kalemia, resulting from a buildup of potassium in the body.
- Tamponade-cardiac, which is the swelling of the pericardium, placing pressure on the heart that is the result of injury or illness.
- Thromboses, including both clots or blockages in the pulmonary or cardiovascular systems.
- Toxins, such as insect and animal bites or other allergens that result in severe distress.
- Tension pneumothorax, which is similar cardiac tamponade, reflecting the build-up of tension in the membrane covering the lungs or the puncture of the lungs and chest wall that equalizes atmospheric and lung pressure, resulting in respiratory distress.
The Future of PALS Megacodes
The lessons learned in the Megacodes simulations should not be taken lightly. The information is presented in a way to increase memory recall, helping trained professionals remember the key steps and interventions in the PALS algorithm. There is no limit to how many times a person may complete the scenarios, and their ease-of-access makes them an ideal way to brush up on PALS skills at any time. If you are still not convinced, consider this; your ability to provide high-quality care to pediatric patients in distress will help keep families together and prevent tragedies. The burden is great, but taking the time to review and improve your skills can make it a little easier to manage.
Have you ever been part of the code team or responded to a child in distress? If so, do you have any tips regarding how to approach providing care for a child who’s panicked, unconscious, or in severe distress? Share your advice and this article to social media now, and remember to put your skills to the test with PALS scenario training today. It’s never too late to learn more about the best ways to increase survival through PALS scenario training.






Leave a Reply