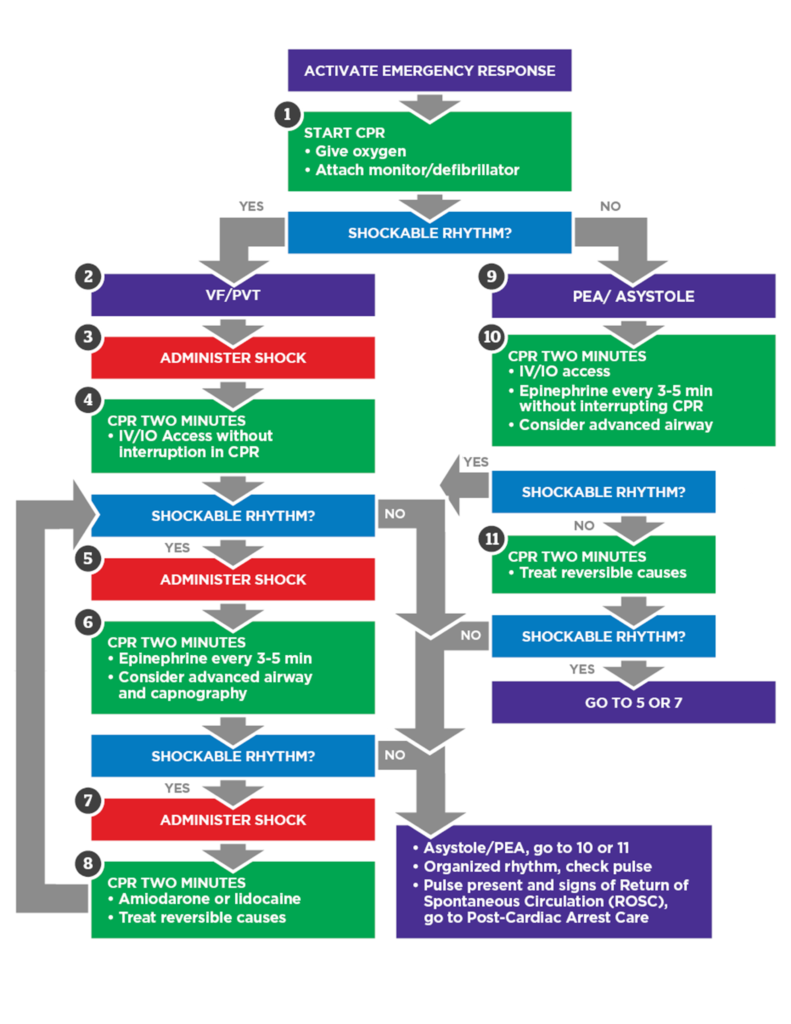
PALS Cardiac Arrest Algorithm
Understanding and effectively implementing the PALS cardiac arrest algorithm is crucial for health care professionals who manage pediatric emergencies. This algorithm provides a structured approach to treating cardiac arrest in infants and children, enhancing the chances of survival and favorable neurological outcomes. In this guide, we will explore the algorithm’s importance, common challenges, and best practices for optimizing patient care.
Importance of the PALS Cardiac Arrest Algorithm
The PALS cardiac arrest algorithm is designed to guide health care providers through the critical steps required during a pediatric cardiac arrest. It emphasizes:
- Early Recognition: Identifying cardiac arrest promptly to initiate immediate intervention.
- High-Quality CPR: Delivering effective chest compressions and ventilations to maintain vital organ perfusion.
- Rapid Defibrillation: Using appropriate energy doses for defibrillation when ventricular fibrillation or pulseless ventricular tachycardia is present.
- Medication Administration: Administering drugs like epinephrine and amiodarone at the correct dosages and intervals.
- Advanced Airway Management: Securing the airway to ensure adequate oxygenation and ventilation.
Adhering to the PALS cardiac arrest algorithm allows providers to make systematic decisions under pressure, improving the likelihood of a successful resuscitation.
Pediatric Cardiac Arrest Algorithm
High-Quality CPR: The Cornerstone of the Algorithm
High-quality CPR is a critical component of the PALS cardiac arrest algorithm. It involves:
- Correct Compression Rate and Depth: 100 to 120 compressions per minute at a depth of one-third the chest diameter (about 1.5 inches/ 4 cm in infants and 2 inches/ 5 cm in children).
- Full Chest Recoil: Allowing the chest to return fully between compressions.
- Minimizing Interruptions: Keeping pauses in compressions under 10 seconds.
- Proper Ventilation: Providing breaths without causing gastric inflation.
Consistent delivery of high-quality CPR improves oxygenation and perfusion to vital organs, which is crucial during cardiac arrest.
Defibrillation and Rhythm Management
For shockable rhythms like ventricular fibrillation (VF) and pulseless ventricular tachycardia (VT), the PALS cardiac arrest algorithm recommends:
- Shock Energy Levels:
- First shock: 2 Joules/kg
- Second shock: 4 Joules/kg
- Subsequent shocks: ≥4 Joules/kg (maximum 10 Joules/kg or adult dose)
- Immediate CPR after each shock, without delaying to reassess the rhythm.
Timely defibrillation can terminate arrhythmias and restore a perfusing rhythm.
Medication Protocols in the Algorithm
Medications are administered according to the PALS cardiac arrest algorithm to support resuscitation efforts:
- Epinephrine:
- IV/IO dose: 0.01 mg/kg (0.1 mL/kg of 1:10,000 concentration)
- Repeat every 3 to 5 minutes
- If IV/IO access is not available, an endotracheal dose of 0.1 mg/kg may be given
- Amiodarone:
- IV/IO dose: 5 mg/kg bolus during cardiac arrest
- May repeat up to two times for refractory VF/pulseless VT
Accurate dosing and timely administration are vital for the effectiveness of these medications.
Addressing Reversible Causes
The PALS cardiac arrest algorithm highlights the importance of identifying and treating reversible causes, known as the “H’s and T’s”:
- H’s:
- Hypovolemia
- Hypoxia
- Hydrogen ion (acidosis)
- Hypothermia
- Hypo-/hyperkalemia
- Hypoglycemia
- T’s:
- Tamponade, cardiac
- Toxins
- Tension pneumothorax
- Thrombosis (pulmonary or coronary)
- Trauma
By promptly addressing these factors, health care providers can correct underlying issues contributing to cardiac arrest.
Enhancing Your Skills with Our Online PALS Certification Course
Continuous education and practice are essential to apply the PALS cardiac arrest algorithm effectively. Enroll in our Online PALS Certification Course to:
- Deepen Your Knowledge: Comprehensive modules covering all aspects of the PALS algorithms.
- Improve Competency: Interactive scenarios to practice critical decision-making.
- Earn Accreditation: Receive a certification recognized by health care institutions nationwide.
- Flexible Learning: Study at your own pace with 24/7 access to course materials.
- Immediate Certification: Obtain your digital certificate upon successful completion.
Take the Next Step in Your Career
Mastery of the PALS cardiac arrest algorithm empowers health care professionals to deliver lifesaving interventions confidently. Regular training and adherence to the algorithm enhance teamwork, streamline resuscitation efforts, and ultimately improve patient outcomes.




