Your cart is currently empty!
Use of any of the ACLS medication in Table 1 should be done within your scope of practice and after a thorough study of the actions and side effects. This table only provides a brief reminder for those who are already knowledgeable in the use of these medications. Moreover, the tablet contains only adult doses, indications, and routes of administration for the most common ACLS drugs.
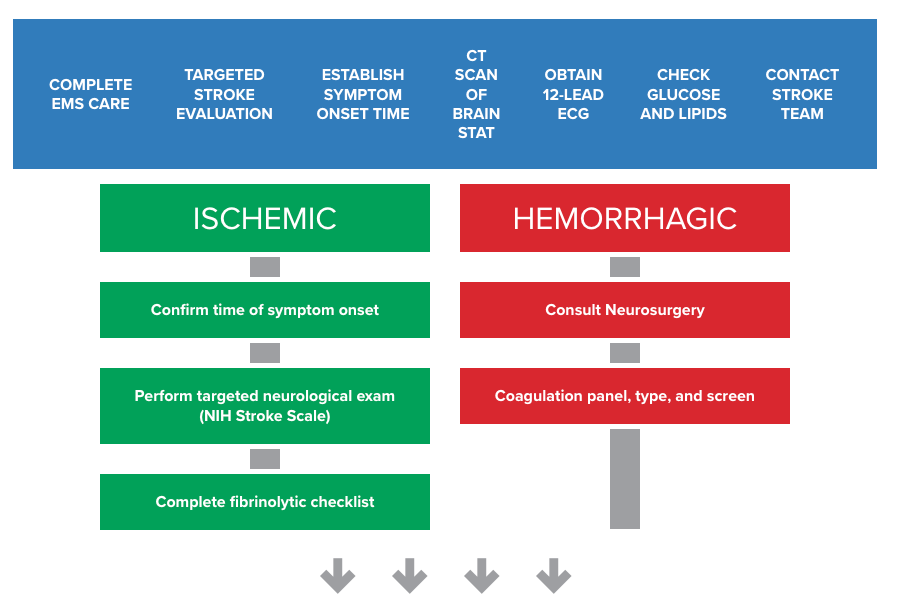
Stroke is a condition in which normal blood flow to the brain is interrupted. Strokes can occur in two variations: ischemic and hemorrhagic. In ischemic stroke, a clot lodges in one of the brain’s blood vessels, blocking blood flow through the blood vessel. In hemorrhagic stroke, a blood vessel in the brain ruptures, spilling blood into the brain tissue. Ischemic stroke and hemorrhagic stroke account for 87% and 13% of the total incidents, respectively. In general, the symptoms of ischemic and hemorrhagic strokes are similar. However, the treatments are very different.
EMS
OXYGEN
FINGERSTICK
HISTORY
EXAM
SEIZURE
IV ACCESS
NOTIFY HOSPITAL
Figure 43
Clinical signs of stroke depend on the region of the brain affected by decreased or blocked blood flow. Signs and symptoms can include: weakness or numbness of the face, arm, or leg, difficulty walking, difficulty with balance, vision loss, slurred or absent speech, facial droop, headache, vomiting, and change in level of consciousness. Not all of these symptoms are present, and the exam findings depend on the cerebral artery affected.
The Cincinnati Prehospital Stroke Scale (CPSS) is used to diagnose the presence of stroke in an individual if any of the following physical findings are seen: facial droop, arm drift, or abnormal speech. Individuals with one of these three findings as a new event have a 72% probability of an ischemic stroke. If all three findings are present, the probability of an acute stroke is more than 85%. Becoming familiar and proficient with the tool FAST utilized by the rescuers’ EMS system is recommended. Mock scenarios and practice will facilitate the use of these valuable screening tools.
FAST: Face Drooping, Arm Weakness, Speech, and Time Symptoms Started
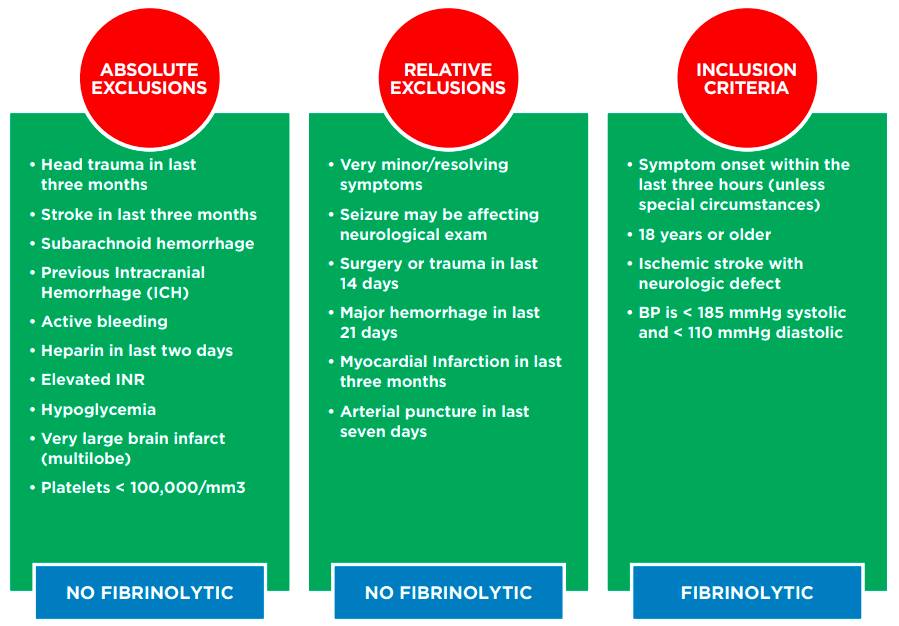
Individuals with ischemic stroke who are not candidates for fibrinolytic therapy should receive aspirin unless contraindicated by true allergy to aspirin. All individuals with confirmed stroke should be admitted to Neurologic Intensive Care Unit if available. Stroke treatment includes blood pressure monitoring and regulation per protocol, seizure precautions, frequent neurological checks, airway support as needed, physical/occupational/speech therapy evaluation, body temperature checks, and blood glucose monitoring. Individuals who received fibrinolytic therapy should be followed for signs of bleeding or hemorrhage. Certain individuals (age 18 to 79 years with mild to moderate stroke) may be able to receive tPA (tissue plasminogen activator) up to 4.5 hours after symptom onset. Under certain circumstances, intra-arterial tPA is possible up to six hours after symptom onset. When the time of symptom onset is unknown, it is considered an automatic exclusion for tPA. If time of symptom onset is known, the National Institute of Neurological Disorders and Stroke (NINDS) has established the time goals below.
10 MINUTES OF ARRIVAL
25 MINUTES OF ARRIVAL
60 MINUTES OF ARRIVAL
180 MINUTES OF ARRIVAL
Figure 44
Before giving anything (medication or food) by mouth, you must perform a bedside swallow screening. All acute stroke individuals are considered NPO on admission.
The goal of the stroke team, emergency physician, or other experts should be to assess the individual with suspected stroke within 10 minutes of arrival in the emergency department (ED).
The CT scan should be completed within 10-25 minutes of the individual’s arrival in the ED and should be read within 45 minutes.