Your cart is currently empty!
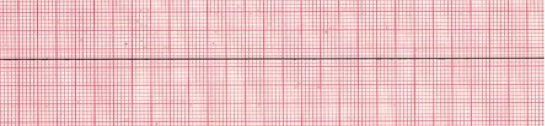
Pulseless electrical activity (PEA) and asystole are related cardiac rhythms in that they are both life-threatening and unshockable cardiac rhythms. Asystole is a flat-line ECG (Figure 27). There may be a subtle movement away from baseline (drifting flat-line), but there is no perceptible cardiac electrical activity. Always ensure that a reading of asystole is not a user or technical error. Make sure pads have good contact with the individual, leads are connected, the gain is set appropriately, and the power is on. PEA is one of many waveforms by ECG (including sinus rhythm) without a detectable pulse. PEA may include any pulseless waveform with the exception of VF, VT, or asystole (Figure 28).
Hypovolemia and hypoxia are the two most common causes of PEA. They are also the most easily reversible and should be at the top of any differential diagnosis.
If the individual has a return of spontaneous circulation (ROSC), proceed to post-cardiac arrest care.
A flatline ECG reveals no electrical activity and is reserved for asystole, whereas PEA reveals organized or semi-organized electrical activity in the absence of a palpable pulse.
| ORGANIZED OR SEMI-ORGANIZED | Any rhythm without a pulse. |
| RATE | Any rate or no rate. |
| P WAVE | Possible P wave or none detectable. |
| PR INTERVAL | Possible PR wave or none detectable. |
| QRS | Possible QRS complex or none detectable. |
| ASYSTOLE REGULARITY | The rhythm will be a nearly flat line. |
| RATE | There is no rate. |
| P WAVE | There are no P waves present. |
| PR INTERVAL | PR interval is unable to be measured due to no P waves being present. |
| QRS | There are no QRS complexes present. |

| REVERSIBLE CAUSES OF CARDIAC ARREST | |
|---|---|
| THE H’S | THE T’S |
| Hypovolemia | Tension pneumothorax |
| Hypoxia | Tamponade |
| H+ (acidosis) | Toxins |
| Hypo/Hyperkalemia | Thrombosis (coronary) |
| Hypoglycemia | Thrombosis (pulmonary) |
| Hypothermia | Trauma (unrecognized) |
Always verify that a reading of asystole is not an equipment failure. Make sure pads make good contact with the individual, all cables are connected, the gain is set appropriately, and the power is on.
Hypovolemia and hypoxia are easily reversed and are the two most common causes of PEA.
Although there is no evidence that atropine has a detrimental effect during bradycardia or asystolic cardiac arrest, routine use of atropine during PEA or asystole has not been shown to have a therapeutic benefit. Therefore, the ILCOR has removed atropine from the cardiac arrest guidelines.
Preliminary research suggested that epinephrine in higher doses may produce improved results in resuscitation. However, research conducted after the 2010 guidelines publication failed to show any benefit over a standard dose of 1 mg epinephrine. Likewise, the 2010 ILCOR guidelines offered an alternative vasopressor, called vasopressin, which could be used instead of or after the first dose of epinephrine. Subsequent research showed that vasopressin offered no benefit over standard-dose epinephrine. Without a demonstration of superiority, both high-dose epinephrine and vasopressin have been removed, simplifying the ACLS algorithm.