Your cart is currently empty!
Understanding normal cardiac anatomy and physiology is an important component of performing ACLS. The heart is a hollow muscle comprised of four chambers surrounded by thick walls of tissue (septum). The atria are the two upper chambers and the ventricles are the two lower chambers. The left and right halves of the heart work together to pump blood throughout the body. The right atrium (RA) and the right ventricle (RV) pump deoxygenated blood to the lungs where it becomes oxygenated. This oxygen-rich blood returns to the left atrium (LA) and then enters the left ventricle (LV). The LV is the main pump that delivers the newly oxygenated blood to the rest of the body.
Blood leaves the heart through a large vessel known as the aorta. Valves between each pair of connected chambers prevent the backflow of blood. The two atria contract simultaneously, as do the ventricles, making the contractions of the heart go from top to bottom. Each beat begins in the RA. The LV is the largest and thickest-walled of the four chambers, as it is responsible for pumping the newly oxygenated blood to the rest of the body.
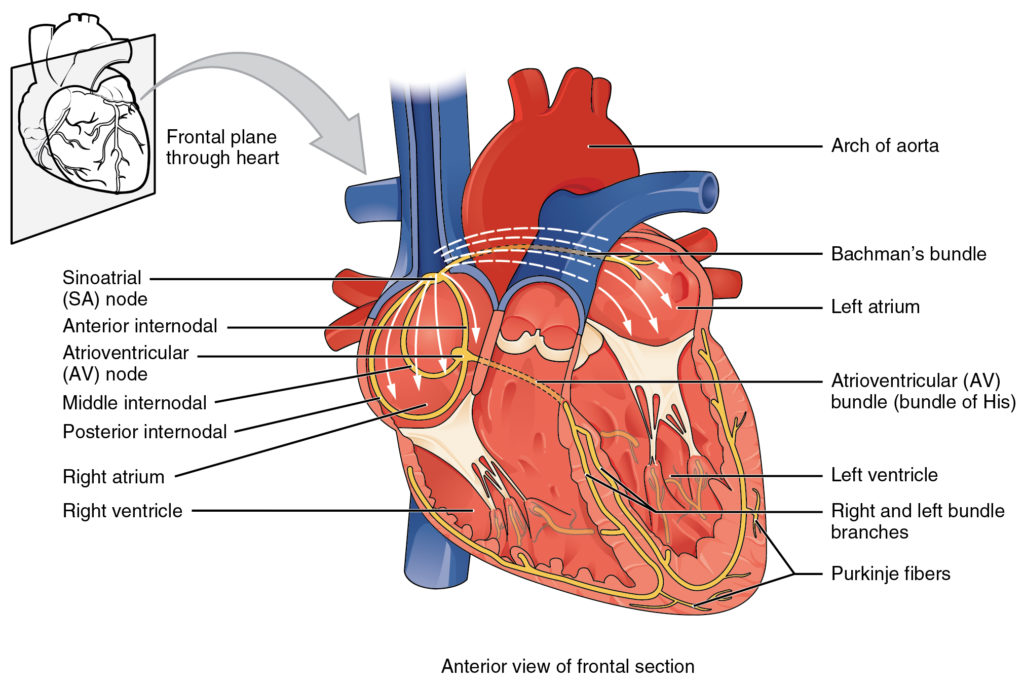
The sinoatrial (SA) node in the RA creates the electrical activity that acts as the heart’s natural pacemaker. This electrical impulse then travels to the atrioventricular (AV) node, which lies between the atria and ventricles (Figure 8a). After pausing there briefly, the electrical impulse moves on to the His–Purkinje system, which acts like wiring to conduct the electrical signal into the LV and RV. This electrical signal causes the heart muscle to contract and pump blood.
By understanding the normal electrical function of the heart, it will be easy to understand abnormal functions. When blood enters the atria of the heart, an electrical impulse that is sent out from the SA node conducts through the atria resulting in atrial contraction.
This atrial contraction registers on an electrocardiogram (ECG) strip as the P wave. This impulse then travels to the AV node, which in turn conducts the electrical impulse through the Bundle of His, bundle branches, and Purkinje fibers of the ventricles causing ventricular contraction. The time between the start of atrial contraction and the start of ventricular contraction registers on an ECG strip as the PR interval. The ventricular contraction registers on the ECG strip as the QRS complex. Following ventricular contraction, the ventricles rest and repolarize, which is registered on the ECG strip as the T wave. The atria also repolarize, but this coincides with the QRS complex, and therefore, cannot be observed on the ECG strip. Together a P wave, QRS complex, and T wave at proper intervals are indicative of normal sinus rhythm (NSR) (Figure 8b), found on next lesson). Abnormalities that are in the conduction system can cause delays in the transmission of the electrical impulse and are detected on the ECG. These deviations from normal conduction can result in dysrhythmias such as heart blocks, pauses, tachycardias and bradycardias, blocks, and dropped beats. These rhythm disturbances will be covered in more detail further in the handbook.