Your cart is currently empty!
Your cart is currently empty!
Advanced Cardiac Life Support (ACLS) Certification Course
ACLS Introduction
The Initial Assessment
ACLS Basic Life Support
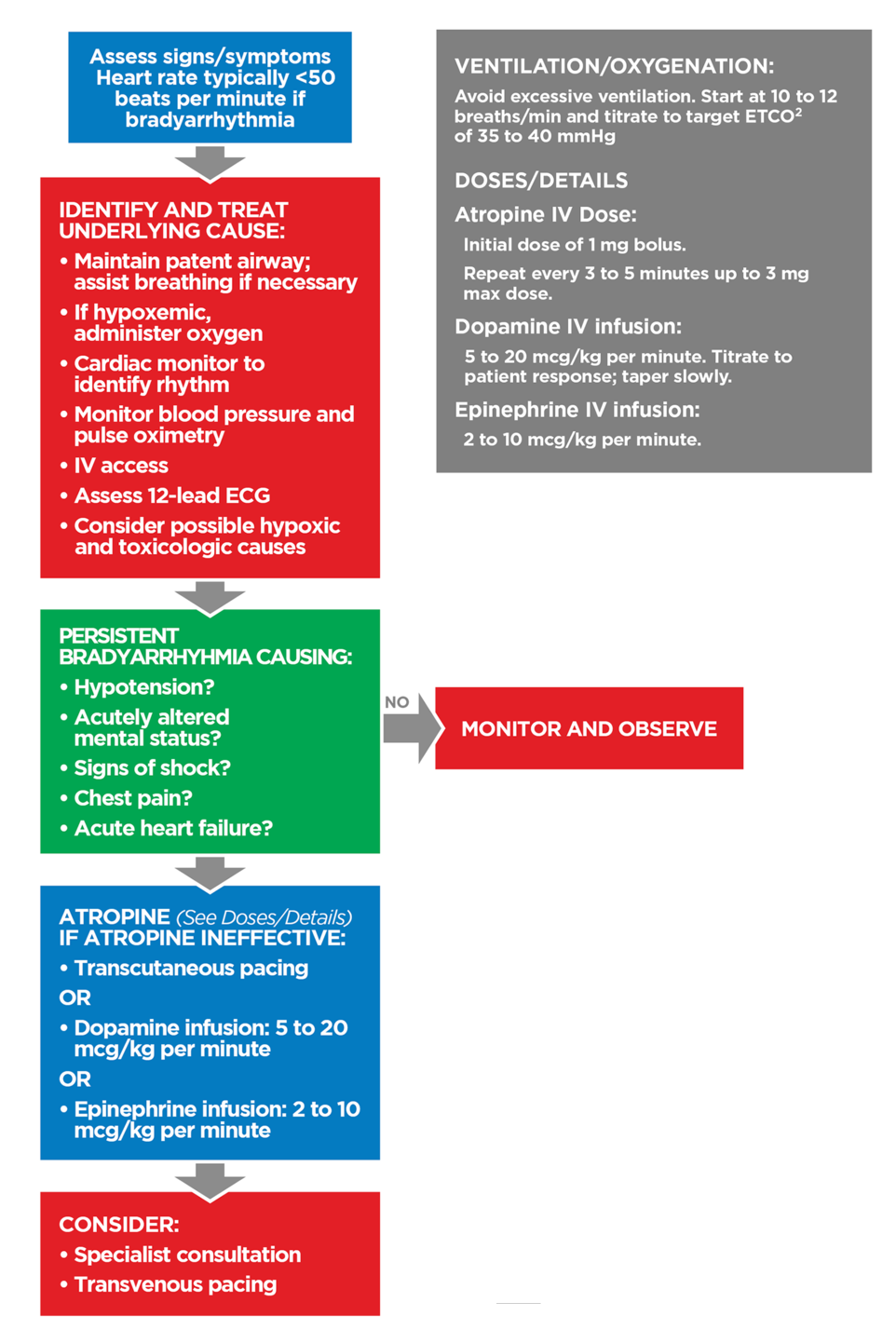
Advanced Cardiac Life Support
Principles of Early Defibrillation
Systems of Care
ACLS Cases
ACLS Skills Training
ACLS Certification Exam
Quick Links
Customer Service
Contact us at
customerservice@savealife.com or
chat with a live agent 24/7
Site Updated:
12/2024
Accreditations
Excellent
4.8 out of 5
